What is heart Transplant?

Heart Transplant is a surgery that removes a diseased heart and replaces it with a healthy heart from a deceased donor to improve your quality of life and increase your life span.
Most heart transplants are done on patients who have end-stage heart failure, a condition in which your heart is severely damaged or weakened, and on people who have failed other treatment options. End-stage heart failure may be caused by conditions such as coronary heart disease, viral infections, or hereditary conditions. In rare instances, a heart transplant may be performed at the same time as lung transplant in patients who have severe heart and lung disease.
Believe it or not, heart transplantation is a relatively simple operation for a cardiac surgeon. In fact, the procedure actually consists of three operations:
The first operation :
It is harvesting the heart from the donor. The donor is usually an unfortunate person who has suffered irreversible brain injury, called “brain death”. Very often these are patients who have had major trauma to the head, for example, in an automobile accident. The victim’s organs, other than the brain, are working well with the help of medications and other “life support” that may include a respirator or other devices.
A team of physicians, nurses, and technicians goes to the hospital of the donor to remove donated organs once brain death of the donor has been determined. The removed organs are transported on ice to keep them alive until they can be implanted. For the heart, this is optimally less than six hours. So, the organs are often flown by airplane or helicopter to the recipient’s hospital.
The second operation :
It is removing the recipient’s damaged heart. Removing the damaged heart may be very easy or very difficult, depending on whether the recipient has had previous heart surgery (as is often the case). If there has been previous surgery, cutting through the scar tissue may prolong and complicate removal of the heart.
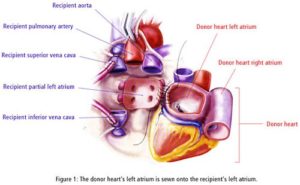
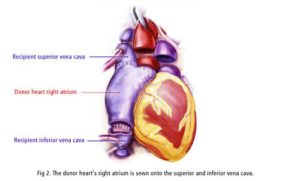
The third operation :
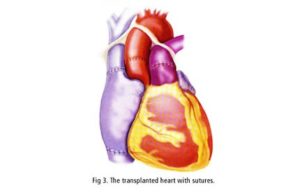
It is probably the easiest; the implantation of the donor’s heart. Today, this operation basically involves the creation of only five lines of stitches, or “anastomoses”. These suture lines connect the large blood vessels entering and leaving the heart. Remarkably, if there are no complications, most patients who have had a heart transplant are home about one week after the surgery. The generosity of donors and their families makes organ transplant possible.
Who needs a heart transplant?
Heart transplants are performed when other treatments for heart problems haven’t worked, leading to heart failure. There are not enough donor hearts available for everyone who may need a heart transplant. Therefore, there is a careful selection process in place to assure that hearts are distributed fairly and to those who will benefit most from the donor’s heart.
Most patients require a transplant because their hearts can no longer pump well enough to supply blood with oxygen and nutrients to the organs of the body. A smaller number of patients have a good pump, but a bad “electrical conduction system” of the heart. That is:
- The rate
- The rhythm
- Sequence of contraction of the heart muscle.
There are all kinds of problems that can occur with the conduction system, including complete interruption of cardiac function causing sudden cardiac death.
Transplants cannot be performed in patients with:
- active infection,
- cancer,
- bad diabetes mellitus;
- patients who smoke or abuse alcohol are also not good candidates.
It’s not easy to be a transplant recipient. These patients need to change their lifestyle and take numerous medications (commonly more than 30 different medications). Hence, all potential transplants patients must undergo psychological testing to identify social and behavioral factors that could interfere with recovery, compliance with medications, and lifestyle changes required after transplantation.
Moreover, needing a heart and being a suitable candidate are not enough. The potential donor heart must be compatible with the recipient’s immune system to decrease the chance of problems with rejection. Finally, this precious resource, the donor organ, must be distributed fairly.
Which type of conditions needs heart Transplant?
The heart transplant in adults is done due to several conditions, including:
- A weakening of the heart muscle (cardiomyopathy).
- Coronary artery disease.
- Heart valve disease.
- A heart problem you’re born with (congenital heart defect).
- Dangerous recurring abnormal heart rhythms (ventricular arrhythmias) not controlled by other treatments.
- Failure of a previous heart transplant.
In children, heart failure is most often caused by either a congenital heart defect or a cardiomyopathy.
Another organ transplant may be performed at the same time as a heart transplant (multiorgan transplant) in people with certain conditions at select medical centers. Which include:
- Heart-kidney transplant: This procedure may be an option for some people with kidney failure in addition to heart failure.
- Heart-liver transplant: This procedure may be an option for people with certain liver and heart conditions.
- Heart-lung transplant: Rarely, doctors may suggest this procedure for some people with severe lung and heart diseases, if the conditions aren’t able to be treated by only a heart transplant or lung transplant.
What are the results of a heart transplant?
When all potential problems are considered, the results of transplantation are remarkably good. Keep in mind that heart failure is a very serious and life-threatening disease. In patients with severe forms of heart failure that require transplantation, the one year mortality rate (that is the percent of patients who die in within one year) is 80%.
Overall, 5-year survival in patients with any form of heart failure is less than 50%. Compare these outcomes with cardiac transplant. After heart transplant, five-year survival averages about 50%-60%. One year survival averages about 85%-90%.
What are the complications of a heart transplant?
As part of our defense mechanism to fight off infection and even cancer, our bodies have an “immune system” to recognize and eliminate foreign tissues such as viruses and bacteria. Unfortunately, our immune system also attacks transplanted organs.
This is what happens when organs are rejected; they are recognized as foreign by the body. Rejection can be controlled with powerful “immunosuppressive” medications. If there is not enough immunosuppression the organ can reject acutely.
Even when it seems that there is no active rejection, there may be subtler chronic rejection that consists of a growth of tissue, something like scar tissue, which causes blockage of the blood vessels of the heart. The blockage of the vessels is the process that ultimately causes the transplanted heart to fail. It is this chronic rejection that is the major limiting factor for the long-term success of heart transplantation.
Unfortunately, immunosuppression is a double-edged sword. While immunosuppression blocks rejection, because it suppresses the immune system, transplant patients are more susceptible to infection and cancers of various types. Among older transplantation patients, as survival has improved, more patients are eventually dying from cancers.
How does a heart transplant patient know if he or she is rejecting the donor organ or developing an infection?
This is not an easy question to answer because many of the symptoms and signs of rejection and infection are the same. These include:
- weakness,
- fatigue,
- malaise (feeling lousy),
- fever,
- Flu-like symptoms, viz, chills, headaches, dizziness, diarrhea, nausea, and/or vomiting.
The more specific symptoms and signs of infection will vary greatly depending upon the site of infection within the body. Transplant patients who experience any of these findings need to seek medical attention immediately. The transplant physician will then do tests to determine whether the transplanted heart is functioning normally or not. If there is no evidence of rejection, a thorough search for infection will be performed so that the patient can be treated appropriately.
Why aren’t more heart transplants done?
It’s not easy to qualify for a heart transplant. One has to have a very bad heart but an otherwise healthy body. However, the major limiting factor is the availability of donor’s hearts. For many reasons, individuals and families refuse to donate organs that could be life-saving to others. Sometimes, even when an organ is available, there is no good match.
Other times, there is no way to get the heart to a suitable recipient in time for the organ to still be viable. Cost is another reason, although less frequent, why more heart transplants aren’t done. The cost is always at least a few hundred thousand dollars. Not all insurers will pay for a heart transplant. The longer the recipient lives, the more expensive the transplant. Of course, if the heart lasts longer, the benefit is also greater to the patient and to society.
