About Prostate Cancer
Prostate cancer is the most common cancer among men in the United States and second most deadly cancer for men. More than 230,000 American men are diagnosed with prostate cancer each year, and more than 29,000 die from the disease annually.
Many men age 50 and older have some trace of prostate cancer. Fortunately, prostate cancer often grows very slowly. When it is detected early, before it has grown beyond the prostate gland, doctors can effectively treat prostate cancer.
A prostate cancer diagnosis is classified according the stage of the cancer. This “staging” relates to where the cancer is in the prostate or outside it.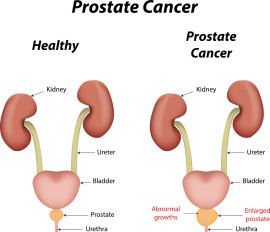
Stage I: The tumour is microscopic. The doctor cannot feel it, but the prostate-specific antigen (PSA) level that indicates potential cancer is elevated.
Stage II: The tumour is limited to within the prostate.
Stage III: The tumour extends outside the prostate.
Stage IV: Cancer has spread to other organs.
More than 90 percent of prostate cancers are detected while they are at stage I, II or III.
Who needs surgery?
Men diagnosed with prostate cancer may be offered surgery, depending on various factors. These include their age, overall health, and the stage of the cancer.
Not everyone who is diagnosed will be treated for prostate cancer, as the treatments come with side effects that can affect quality of life.
Because prostate cancer grows slowly, doctors may recommend watchful waiting or active surveillance, if the condition is not causing any symptoms. Watchful waiting or active surveillance mean being monitored closely for signs that the cancer is growing. Treatment will only be offered if and when it is necessary.
Causes of prostate cancer
Like other cancers, prostate cancer develops when some cells in the prostate mutate or become abnormal. These cells grow and divide faster than normal cells, forming a tumour. Some cancer cells might metastasize, or spread to other parts of the body.
The exact cause of prostate cancer is unknown. However, researchers have identified certain risk factors for prostate cancer including:
- Being older than age 50. The risk of prostate cancer increases with age; about 80 percent of prostate cancer occurs in men older than age 65.
- Living in North America and Northern Europe. Prostate cancer occurs more frequently in these areas than in other parts of the world.
- Being of African-American heritage. African-American men are more likely to get prostate cancer, and their death rate from prostate cancer is higher.
- Having a family history of prostate cancer or breast cancer.
- Being obese. Research has linked obesity and increased risk of death from prostate cancer.
- Eating a diet high in fat and/or red meat. Studies suggesting this risk factor may not be definitive, but men who eat a diet higher in fat appear to have more risk of prostate cancer. A fattier diet also might raise the levels of hormones that cause prostate cancer to grow faster.
Symptoms of prostate cancer
Many men who have prostate cancer are unaware they have it. Prostate cancer usually grows very slowly and might not cause symptoms at first. Prostate enlargement and prostate cancer often share similar symptoms. It is important to be aware of the symptoms in order to seek a prompt medical evaluation. The cancer can be very dangerous if it spreads outside the prostate or begins to grow faster.
Prostate cancer that is growing might cause symptoms such as:
- Needing to urinate often, especially at night
- Weaker stream of urine or trouble urinating
- Difficulty starting or stopping urine
- Pain or burning during urination or ejaculation
- Blood in urine or semen
- Inability to urinate standing up
- Leaking urine when you laugh or cough
- Pelvic pain or discomfort
- Erectile dysfunction
Advanced prostate cancer, or stage IV prostate cancer that has spread to other parts of the body, might cause additional symptoms such as: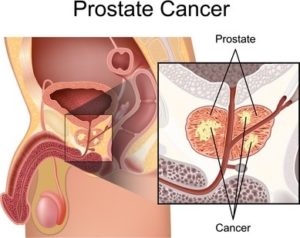
- Pain in the bones of the pelvis or lower body
- Dull, deep pain or stiffness in the pelvis or upper thighs, lower back or ribs
- Losing weight or reduced appetite
- Fatigue, nausea, vomiting or constipation
- Swelling of the legs and feet
- A sense of weakness, or even paralysis, in the legs (constipation sometimes accompanies this weakness).
Men who experience any of these symptoms should contact their doctor.
Diagnosis of prostate cancer
Experts continually debate how and how frequently doctors should screen men for prostate cancer. Medical organizations are still reviewing which patients benefit most from screening and treatment for this disease.
Screening and diagnosis can have their own risks. These include false-negatives, false positives and “over diagnosis,” meaning a cancer that would never have caused any problem is detected and treated, unnecessarily placing the patient at risk from radiation or surgery. Physicians help each patient determine whether screening makes sense for him.
Initial screening
Doctors screen men for prostate cancer in two primary ways:
- Prostate-specific antigen (PSA) test. A laboratory examines a blood sample for PSA. If the level of PSA is higher than normal, it could indicate a problem with the prostate.
- Digital rectal exam (DRE). A DRE is a manual exam in which the doctor inserts a gloved finger into the rectum to feel the prostate. Because the prostate is next to the rectum, the doctor can note anything unusual.
Doctors cannot feel very small tumours. For that reason, a PSA test is more reliable for very early prostate cancer. For 85 percent of men with prostate cancer, the cancer is caught early. The outlook for these patients is good.
Further testing
If your doctor suspects that a patient might have a prostate abnormality, he or she may order additional tests. These might include:
Ultrasound: Ultrasound testing uses a small probe, about the size of a finger, inserted in the rectum. The ultrasound wand uses sound waves to make a picture of the prostate gland for experts to examine.
Biopsy: Through a thin needle, a physician collects a sample of tissue from the prostate gland. A laboratory analyzes the sample to determine whether cancer cells are growing in the prostate.
If these tests indicate cancer is present, the patient will be assigned a Gleason score. The Gleason score is a scale based on the results of the blood test and how biopsied tissue looks. It is a way for physicians to understand how aggressive the cancer might be and helps them in assessing the stage of the prostate cancer.
For cancers that are more advanced, doctors will order more tests to find out if the cancer has spread within the body. These tests might include:
- Computerized tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Bone scan
Treatment of prostate cancer
Positron emission tomography (PET) scan.
Not every patient needs to have all of these tests. Doctors will tell patients which tests are right for them.
Treatment options will be different for each patient, depending on the stage of the cancer, the age of the patient and other factors. The treatments for prostate cancer page provide more details about the variety of available treatments, some of which are listed below.
Observing detected cancer but providing no treatment is often called “watchful waiting” or “active surveillance.” The major flaw in this approach is that men don’t return to see their doctor for updated surveillance.
- Hormone therapy to stop the body from producing testosterone, which cancer cells rely on for growth.
- Radiation therapy, Cyber knife/SBRT, external beam or internal insertions of radioactive seeds that deliver radiation (brachytherapy).
- Surgery to remove the prostate. This can be done laparoscopic of robotically with small incisions or using the traditional open approach.
Types of prostate cancer surgery
There are two main types of prostate cancer surgery: radical prostatectomy and transurethral resection of the prostate (TURP).
Radical prostatectomy
A radical prostatectomy may be offered to men with localized prostate cancer who are otherwise fit and healthy. If the cancer has spread outside of the prostate, this operation may not be suitable.
During a radical prostatectomy, the whole prostate gland, and the cancer within it, is removed. The seminal vesicles are also taken out, along with the nearby lymph nodes, if there is a risk the cancer may have spread to them.
The type of radical prostatectomy performed will depend on the hospital.
Laparoscopy is carried out by making several small cuts into the abdomen and removing the prostate.
Keyhole surgery, also called a laparoscopy or minimally invasive surgery, involves the surgeon making five or six cuts in the abdomen to remove the prostate. This is done by hand with the surgeon guided by a camera and lighted tube.
In robot-assisted surgery, the surgeon uses three robotic arms controlled from a computer.
During open surgery or retro pubic prostatectomy, a single cut is made in the stomach. A less common form of open surgery is a perinea prostatectomy. This is when a cut is made between the testicles and the back passage.
Risks
As with all surgery, the removal of the prostate gland carries risks. These include:
- Bleeding
- injury to nearby organs such as bowel and nerves
- blood clots
- infection
- Side effects
The most common side effects are leaking urine, known as urinary incontinence, and difficulty getting or keeping an erection, known as erectile dysfunction.
After surgery, most men cannot control their bladder properly. Some may experience stress incontinence, which means leaking just a few drops of urine during exercise, coughing, or sneezing. Others may need absorbent pads or pants, though this usually improves with time.
Some men have difficulty urinating after the operation, and this can happen gradually or very suddenly.
Most men who have this kind of surgery suffer erectile dysfunction. Surgeons will try to save the nerves that control erections, but this is not always possible. Even if nerves are saved, many men still have difficulty with erections.
It can take between a few months and 3 years for erections to return, but some men will always need help or medication.
TURP
A TURP operation does not cure the cancer. It helps with one of the most common symptoms of prostate cancer, which is difficulty passing urine. This happens when the enlarged prostate presses against the urethra, causing it to narrow.
It is carried out under general anaesthesia and involves a surgeon passing a thin metal tube with a camera on the end through the penis to the urethra.
A small wire loop is then put through the tube and heat is used to remove small parts of prostate tissue. During the operation, fluid is passed through the bladder to flush away the removed tissue.
Banking sperm is one option for men who would like to father children after their operation.
Possible side effects of TURP include:
- problems urinating, though this usually improves over time
- stress incontinence, affecting around 2 percent of patients
- blood in urine for the first couple of weeks after the procedure
- urine infection
- slow urine flow caused by scar tissue from the operation, affecting 4 percent of patients
- erectile dysfunction, affecting up to 7 percent of patients
Around 65 percent of men will suffer retrograde ejaculation. This means that semen is passed into the bladder during orgasm rather than being ejaculated.
Men who have retrograde orgasm experience orgasm differently and may not be able to father children through sex. Banking sperm is a treatment option for this side effect.
