Introduction about Gastro –Intestinal Surgery
Gastric bypass surgery combines the creation of a small stomach pouch to restrict food intake and construction of bypasses of the duodenum and other segments of the small intestine to cause malabsorption (decreased ability to absorb calories and nutrients from food).
Gastroenterological surgery includes a variety of surgical procedures performed on the organs and conduits of the digestive system. These procedures include the repair, removal, or resection of the oesophagus, liver, stomach, spleen, pancreas, gallbladder, colon, anus, and rectum. Gastroenterology surgery is performed for diseases ranging from appendicitis, gastroesophageal reflux disease (GERD), and gastric ulcers to the life-threatening cancers of the stomach, colon, liver, and pancreas, and ulcerative conditions like ulcerative colitis and Cohn’s disease.
Purpose
Scientific understanding, treatment, and diagnostic advances, combined with an aging population, have made this century the golden age of gastroenterology. Gasteroenterologic surgery’s success in treating conditions of the digestive system by removing obstructions, diseased or malignant tissue, or by enlarging and augmenting conduits for digestion is now largely due to the ability to view and work on the various critical organs through video representation and by biopsy. The word abdomen is derived from the Latin abdere , meaning concealed or un-seeable. The use of gastrointestinal endoscopy, laproscopy, computer tomography (CT) scan, and ultrasound has made the inspection of inaccessible organs possible without surgery, and so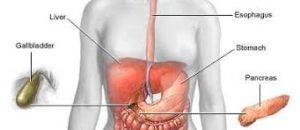 metimes treatable with only minor surgery. With advances in other diagnostics such as the faecal occult blood test known as the Guaiac test, the need for bowel surgery can be determined quickly without expensive tests. This is especially important for colon cancer, which is the leading cause of cancer mortality in the United State, with about 56,000 Americans dying from it each year.
metimes treatable with only minor surgery. With advances in other diagnostics such as the faecal occult blood test known as the Guaiac test, the need for bowel surgery can be determined quickly without expensive tests. This is especially important for colon cancer, which is the leading cause of cancer mortality in the United State, with about 56,000 Americans dying from it each year.
Some prominent surgical procedures included in gasteroentologic surgery are:
- Fundoplication to prevent reflux acids in the stomach from damaging the esophagus.
- Appendectomy for removal of an inflamed or infected appendix.
- Cholecystectomy for removal of an inflamed gallbladder and the crystallized salts called gallstones.
- Vagotomy, antrectomy , pyloroplasty are surgeries for gastric and peptic ulcers, now very rare. In the last 10 years, medical research has confirmed that gastric and peptic ulcers are due primarily to Heliobacter pylori , which causes more than 90% of duodenal ulcers and up to 80% of gastric ulcers. The most frequent surgeries today for ulcers of the stomach and duodenum are for complications of ulcerative conditions, largely perforation.
- Colostomy , ileostomy , and ileoanal reservoir surgery are done to remove part of the colon by colostomy; part of the colon as it enters the small intestine by ileostomy; and rem
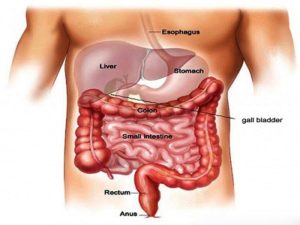 oval of part of the colon as it enters the rectal reservoir by ileonal reservoir surgery. These surgeries are required to relieve diseased tissue and allow for the continuation of waste to be removed from the body. Inflammatory bowel disease includes two severe conditions: ulcerative colitis and Crohn’s disease. In both cases, portions of the bowel must be resected. Crohn’s disease affects the small intestine and ulterative colitis affects the lining of the colon. Cancers in the area of the colon and rectum can also necessitate the resection of the colon, intestine, and/or rectum.
oval of part of the colon as it enters the rectal reservoir by ileonal reservoir surgery. These surgeries are required to relieve diseased tissue and allow for the continuation of waste to be removed from the body. Inflammatory bowel disease includes two severe conditions: ulcerative colitis and Crohn’s disease. In both cases, portions of the bowel must be resected. Crohn’s disease affects the small intestine and ulterative colitis affects the lining of the colon. Cancers in the area of the colon and rectum can also necessitate the resection of the colon, intestine, and/or rectum.
Types of Gastric Bypass Surgery
Roux-en-Y gastric bypass (RGB): This operation is the most common gastric bypass surgery performed in the U.S. First, a small stomach pouch is created by stapling part of the stomach together or by vertical banding. This limits how much food you can eat. Next, a Y-shaped section of the small intestine is attached to the pouch to allow food to bypass the duodenum as well as the first portion of the jejunum. This causes reduced calorie and nutrient absorption. This procedure can now be done with a laparoscope (a thin telescope-like instrument for viewing inside the abdomen) in some people. This involves using small incisions and generally has a more rapid recovery time.
Extensive gastric bypass (biliopancreatic diversion): In this more complicated gastric bypass operation, the lower portion of the stomach is removed. The small pouch that remains is connected directly to the final segment of the small intestine, thus completely bypassing both the duodenum and jejunum. Although this procedure successfully promotes weight loss, it is not as widely used because of the high risk for nutritional deficiencies.
Gastric bypass surgery that causes malabsorption and restricts food intake produces more weight loss than restriction operations like gastric banding, which only decrease food intake. People who have bypass surgery generally lose two-thirds of their excess weight within two years.
Risks of Gastric Bypass Surgery
People who undergo gastric bypass surgery are at risk for:
- Pouch stretching (stomach gets bigger overtime, stretching back to its original size).
- Band erosion (the band closing off part of the stomach disintegrates).
- Breakdown of staple lines (band and staples fall apart, reversing the procedure).
- Leakage of stomach contents into the abdomen (this is dangerous because the acid can eat away other organs).
- Nutritional deficiencies causing health problems.
Gastric bypass surgery also may cause “dumping syndrome,” whereby stomach contents move too rapidly through the small intestine. Symptoms include nausea, weakness, sweating, faintness, and, occasionally, diarrhoea after eating, as well as the inability to eat sweets without becoming extremely weak. Gallstones can occur in response to rapid weight loss. They can be dissolved with medication taken after the surgery.
Description
Advances in laparoscopy allow the direct study of large portions of the liver, gallbladder, spleen, lining of the stomach, and pelvic organs. Many biopsies of these organs can be performed by laparoscopy. Increasingly, laparoscopic surgery is replacing open abdomen surgery for many diseases, with some procedures performed on an outpatient basis. Gastrointestinal applications have resulted in startling changes in surgeries for appendectomy, gallbladder, and adenocarcinoma of the oesophagus, the fastest increasing cancer in North America. Significant other diseases include liver, colon, stomach, and pancreatic cancers; ulcerative conditions in the stomach and colon; and inflammations and/or irritations of the stomach, liver, bowel, and pancreas that cannot be treated with medications or other therapies. Recent research has shown that laparoscopy is useful in detecting small (< 0.8 in [< 2 cm]) cancers not seen by imaging techniques and can be used to stage pancreatic or oesophageal cancers, averting surgical removal of the organ wall in a high percentage of cases. There are also recent indications, however, that some laparoscopic procedures may not have the long-lasting efficacy of open surgeries and may involve more complications. This drawback has proven true for laparoscopic fundoplication for GERD disease.
Advances in gastrointestinal fiber-optic endoscopic technology have made endoscopy mandatory for gastrointestinal diagnosis, therapy, and surgery. Especially promising is the use of endoscopic techniques in the diagnosis and treatment of bowel diseases, colonoscopy, and sigmoidoscopy , particularly with acute and chronic bleeding. Combined with laparoscopic techniques, endoscopy has substantially reduced the need for open surgical techniques for the management of bleeding.
For most gasteroenterologic surgeries, whether laparoscopic or open, preoperative medications are given as well as general anesthesia. Food and drink are not allowed after midnight before the surgery the next morning. Surgery proceeds with the patient under general anesthetics for open surgery and local or regional anesthetics for laparoscopic surgery. Specific diseases require specific procedures, with resection and repair of abdomen, colon and intestines, liver, and pancreas considered more serious than other organs. The level of complication of the procedure dictates whether laparoscopic procedures may be used.
Gastric bypass is major surgery and it has many risks. Some of these risks are very serious. You should discuss these risks with your surgeon.
Risks for anaesthesia and surgery in general include:
- Allergic reactions to medicines
- Breathing problems
- Bleeding, blood clots, infection
During the week before your surgery:
- You may be asked to stop taking medicines that make it hard for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), vitamin E, warfarin (Coumadin), and others.
- Ask your doctor who drugs you should still take on the day of your surgery.
- Prepare your home for after the surgery.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the drugs your doctor told you to take with a small sip of water.
- Arrive at the hospital on time.
- Gastritis (inflamed stomach lining), heartburn, or stomach ulcers
- Injury to the stomach, intestines, or other organs during surgery
- Leaking from the line where parts of the stomach have been stapled together
- Poor nutrition
- Scarring inside your belly that could lead to a blockage in your bowel in the future
- Vomiting from eating more than your stomach pouch can hold
Complications from Nutritional Deficiencies
The limited absorption of vitamin B-12 and iron can cause anaemia. The lack of calcium absorption can cause osteoporosis and metabolic bone disease. People who undergo this procedure are required to take nutritional supplements that usually prevent these deficiencies.
The more extensive the gastric bypass surgery, the greater the risk for complications and nutritional deficiencies. People who undergo extensive bypasses of the normal digestive process require not only close monitoring, but also lifelong use of special foods and medications.
What Can I Expect After Gastric Bypass Surgery?
For the first month, you will only be able to handle small amounts of soft food and liquids. But gradually, you will be able to add solid foods back into your diet. You will notice feeling full very quickly – after eating about two tablespoons of food. Your physician may also recommend that you take nutritional supplements.
Within the first two years, you can expect to lose one-half to two-thirds of your excess body weight. Weight loss will continue, in most cases, for a year and a half before stabilizing.
At UCLA, our specialists will work with both you and your primary care physician to make sure your recovery is as smooth as possible.
Advantages of the Gastric Bypass
It is particularly effective for patients with a larger BMI as the procedure has more predictable weight loss outcomes.
Hormonal changes resulting from surgery mean most patients have an almost immediate reduction in their need for diabetic medication, and some can completely stop diabetic medication altogether.
In addition to weight loss, gastric Bypass tends to have the strongest effect on high blood pressure, high cholesterol, and other obesity-related health issues.
It is also effective for those people who tend towards high sugar or high-fat foods. Dumping syndrome is directly linked to a high sugar, high fat intake. Symptoms of dumping are unpleasant and therefore discourage the intake of high calorie, sweet foods.
