Brief about Liver Transplantation
A liver transplant is an operation that replaces a patient’s diseased liver with a whole or partial healthy liver from another person. This article explains the current indications for liver transplantation, types of donor livers, the operation itself, and the immunosuppressant that is required after transplantation.
A liver transplant is an operation that replaces a patient’s diseased liver with a whole or partial healthy liver from another person. This article explains the current indications for liver transplantation, types of donor livers, the operation itself, and the immunosuppressant that is required after transplantation.
Description:
Liver transplantation is surgery that is performed to remove a diseased liver in order to replace it with a healthy one. Such surgeries have been done for over 38 years. Several people who have had liver transplants go on to lead perfectly normal lives.
The donated liver may be from:
A donor who has recently died and has not had liver injury. This type of donor is called a cadaver donor.
Sometimes, a healthy person will donate part of his or her liver to a person with a diseased liver. For example, a parent may donate to a child. This kind of donor is called a living donor. The liver can regrow itself. Both people most often end up with fully working livers after a successful transplant.
The donor liver is transported in a cooled salt-water (saline) solution that preserves the organ for up to 8 hours. The necessary tests can then be done to match the donor with the recipient.
The new liver is removed from the donor through a surgical cut in the upper abdomen. It is placed into the person who needs the liver (called the recipient), and attached to the blood vessels and bile ducts. The operation may take up to 12 hours. The recipient will often need a large amount of blood through a transfusion.
Your liver is your largest internal organ and performs several critical functions, including:
- Removing bacteria and toxins from the blood
- Preventing infection and regulating immune responses
- Processing nutrients, medications and hormones
- Producing bile, which helps the body absorb fats, cholesterol and fat-soluble vitamins
- Making proteins that help the blood clot
- Liver transplant is usually reserved as a treatment option for people who have significant complications due to end-stage chronic liver disease. In rare cases, sudden failure of a previously normal liver may occur.
When does one require a liver transplant?
Liver disease severe enough to require a liver transplant can come from many causes. In adults, the most common reason for liver transplantation is cirrhosis. Cirrhosis is a condition in which the liver slowly deteriorates and malfunctions due to chronic injury. Scar tissue replaces healthy liver tissue, partially blocking the flow of blood through the liver. Cirrhosis can be caused by viruses such as hepatitis B and C, alcohol, autoimmune liver diseases, build-up of fat in the liver, and hereditary liver diseases. Many people who develop cirrhosis of the liver due to excessive use of alcohol also need a liver transplant. Abstinence from alcohol and treatment of complications for 6 months will usually allow some of them to improve significantly and these patients may survive for prolonged periods without a transplant. For patients with advanced liver disease, where prolonged abstinence and medical treatment fails to restore health, liver transplantation is the treatment.
In children, the most common reason for liver transplantation is biliary atresia. Biliary atresia is a rare condition in newborn infants in which the common bile duct between the liver and the small intestine is blocked or absent. Bile ducts, which are tubes that carry bile out of the liver, are missing or damaged in this disease, and obstructed bile causes cirrhosis. Bile helps digest food. If unrecognised, the condition leads to liver failure. The cause of the condition is unknown. The only effective treatments are certain surgeries, or liver transplantation.
Other reasons for transplantation are liver cancer, benign liver tumours, an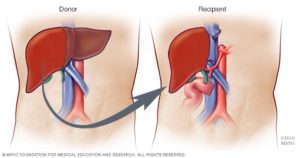 d hereditary diseases. Primary liver cancers develop at a significantly higher rate in cirrhotic livers as compared to normal livers, particularly in patients having liver disease secondary to Hepatitis B. Liver Transplantation at an early stage of liver cancer may result in long-term survival for select patients. However, cancers of the liver that begin somewhere else in the body and spread to the liver are not curable with a liver transplant.
d hereditary diseases. Primary liver cancers develop at a significantly higher rate in cirrhotic livers as compared to normal livers, particularly in patients having liver disease secondary to Hepatitis B. Liver Transplantation at an early stage of liver cancer may result in long-term survival for select patients. However, cancers of the liver that begin somewhere else in the body and spread to the liver are not curable with a liver transplant.
How are candidates for liver transplant determined?
Evaluations by specialists from a variety of fields are needed to determine if a liver transplant is appropriate. The evaluation includes a review of your medical history and a variety of tests. The transplant team will arrange blood tests, X – rays, and other tests to help make the decision about whether you need a transplant and whether a transplant can be carried out safely. Other aspects of your health-like your heart, lungs, kidneys, immune system, and mental health-will also are checked to be sure you’re strong enough for surgery.
The Liver Transplant Operation
A liver transplant involves the removal of and preparation of the donor liver, removal of the diseased liver, and implantation of the new organ. The liver has several key connections that must be re-established for the new organ to receive blood flow and to drain bile from the liver. The structures that must be reconnected are the inferior vena cava, the portal vein, the hepatic artery, and the bile duct. The exact method of connecting these structures varies depending on specific donor and anatomy or recipient anatomic issues and, in some cases, the recipient disease.
For someone undergoing liver transplantation, the sequence of events in the operating room is as follows:
- Incision
- Evaluation of the abdomen for abnormalities that would preclude liver transplantation (for example: undiagnosed infection or malignancy)
- Mobilization of the native liver (dissection of the liver attachments to the abdominal cavity)
- Isolation of important structures (the inferior vena cava above, behind, and below the liver; the portal vein; the common bile duct; the hepatic artery)
- Tran section of the above mentioned structures and removal of the native, diseased liver.
- Sewing in the new liver: First, venous blood flow is re-established by connecting the donor’s and the recipient’s inferior vena cava and portal veins. Next, arterial flow is re-established by sewing the donors and recipients hepatic arteries. Finally, biliary drainage is achieved by sewing the donor’s and recipient’s common bile ducts.
- Ensuring adequate control of bleeding
- Closure of the incision
Your health care provider will refer you to a transplant centre. The transplant team will want to make sure that you are a good candidate for a liver transplant. You will make a few visits over several weeks or months. You will need to have blood drawn and x-rays taken.
If you are the person getting the new liver, the following tests will be done before the procedure:
- Tissue and blood typing to make sure your body will not reject the donated liver
- Blood tests or skin tests to check for infection
- Heart tests such as an EKG, echocardiogram, or cardiac catheterization
- Tests to look for early cancer
- Tests to look at your liver, gallbladder, pancreas, small intestine, and the blood vessels around the liver
- Colonoscopy, depending on your age
You may choose to look at one or more transplant centres to determine which is best for you:
- Ask the centre how many transplants they perform every year, and their survival rates. Compare these numbers to those of other transplant centres.
- Ask what support groups they have available, and what travel and housing arrangements they offer.
If the transplant team thinks you are a good candidate for a liver transplant, you will be put on a national waiting list.
Your place on the waiting list is based on a number of factors. Key factors include the type of liver problems you have, how severe your disease is, and the likelihood that a transplant will be successful.
The amount of time you spend on a waiting list is most often not a factor in how soon you get a liver, with the possible exception of children.
While you are waiting for a liver, follow these steps:
- Follow any diet your transplant team recommends.
- Do not drink alcohol.
- Do not smoke.
- Keep your weight in the appropriate range. Follow the exercise program your provider recommends.
- Take all medicines prescribed for you. Report changes in your medicines and any new or worsening medical problems to the transplant team.
- Follow-up with your regular provider and transplant team at any appointments that have been made.
- Make sure the transplant team has your correct phone numbers, so they can contact you immediately if a liver becomes available. Make sure that, no matter where you are going, you can be contacted quickly and easily.
- Have everything ready ahead of time to go to the hospital.
After the Procedure
If you received a donated liver, you will likely need to stay in the hospital for a week or longer. After that, you will need to be closely followed up by a doctor for the rest of your life. You will have regular blood tests after the transplant.
The recovery period is about 6 to 12 months. Your transplant team may ask you to stay close to the hospital for the first 3 months. You will need to have regular check-ups, with blood tests and x-rays for many years.
Complications
Two of the most common complications following liver transplant are rejection and infection.
Rejection:
Your immune system works to destroy foreign substances that invade the body. But the immune system can’t distinguish between your transplanted liver and unwanted invaders, such as viruses and bacteria. So, your immune system may attempt to attack and destroy your new liver. This is called a rejection episode. About 64% of all liver-transplant patients have some degree of organ rejection, most within the first 90 days of transplant. Anti-rejection medications are given to ward off the immune attack.
Infection:
Because anti-rejection drugs that suppress your immune system are needed to prevent the liver from being rejected, you are at higher risk for infections. This problem lessens as time passes. Not all patients have problems with infections, and most infections can be treated successfully as they happen.
Recovery:
Initially in the intensive care unit there is very careful monitoring of all body functions, including the liver. Once the patient is transferred to the ward, the frequency of blood testing, etc. is decreased, eating is allowed and physiotherapy is prescribed to regain muscle strength. The drug or drugs to prevent rejection are initially given by vein, but later by mouth. During the transplantation, frequent tests are done to monitor liver function and detect any evidence of rejection.
Do immunosuppressants have any side effects?
Immunosuppressant drugs lower a person’s resistance to infection and can make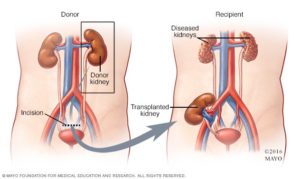 infections harder to treat. Although these medications are meant to prevent rejection of the liver, they also decrease the ability of the body to fight off certain viruses, bacteria, and fungi. The organisms that most commonly affect patients are covered with preventive medications. However, avoiding contact with people who have infections is very important.
infections harder to treat. Although these medications are meant to prevent rejection of the liver, they also decrease the ability of the body to fight off certain viruses, bacteria, and fungi. The organisms that most commonly affect patients are covered with preventive medications. However, avoiding contact with people who have infections is very important.
Can anyone with liver problems get a transplant?
You cannot have a transplant if you have:
- cancer in another part of your body
- serious heart,
- lung, or nerve disease active alcohol or illegal drug abuse an active,
- Severe infection inability to follow your doctor’s instructions.
