Shoulder Replacement: A short Description
The shoulder is a ball and socket joint. The round end of the arm bone fits into the opening at the end of the shoulder blade, called the socket. This type of joint allows you to move your arm in most directions.
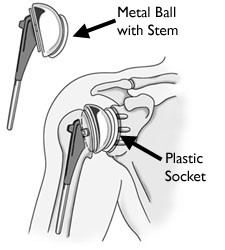
In shoulder replacement surgery, the damaged parts of the shoulder are removed and replaced with artificial components, called prosthesis. The treatment options are either replacement of just the head of the humerus bone (ball), or replacement of both the ball and the socket (glenoid).
For total shoulder replacement, the round end of your arm bone will be replaced with an artificial stem that has a rounded metal head. The socket part (glenoid) of your shoulder blade will be replaced with a smooth plastic shell (lining) that will be held in place with special cement. If only 1 of these 2 bones needs to be replaced, the surgery is called a partial shoulder replacement, or a hemiarthroplasty.
For shoulder joint replacement, your surgeon will make an incision (cut) over your shoulder joint to open up the area. Then your surgeon will:
- Remove the head (top) of your upper arm bone (humerus)
- Cement the new metal head and stem into place
- Smooth the surface of the old socket and cement the new one in place
- Close your incision with staples or sutures
- Place a dressing (bandage) over your wound
- Your surgeon may place a tube in this area to drain fluid that may build up in the joint. The drain will be removed when you no longer need it.
- This surgery normally takes 1 to 3 hours.
Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle). The shoulder is a ball-and-socket joint: The ball, or head, of your upper arm bone fits into a shallow socket in your shoulder blade. This socket is called the glenoid.
The surfaces of the bones where they touch are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily. A thin, smooth tissue called synovial  membrane covers all remaining surfaces inside the shoulder joint. In a healthy shoulder, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost any friction in your shoulder.
membrane covers all remaining surfaces inside the shoulder joint. In a healthy shoulder, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost any friction in your shoulder.
The muscles and tendons that surround the shoulder provide stability and support.
All of these structures allow the shoulder to rotate through a greater range of motion than any other joint in the body.
Procedure:
The surgeon begins by separating the deltoid and pectoral muscles, accessing the shoulder in a largely nerve-free area to minimize nerve damage. The shoulder is covered by the rotator cuff, which must be opened by cutting one of the anterior (front) rotator cuff muscles. This “opens the door,” allowing the surgeon to view and manipulate the arthritic parts of the shoulder ball and socket.
After the arthritic sections have been removed, the surgeon inserts the implant socket, ball, and stem components, closes and stitches the rotator cuff muscle, and stitches and cleans the incision, after which a bandage is applied as a temporary covering.
The surgical procedure
- The shoulder is approached from either the front (deltopectoral), or from the side (deltoid split).
- The choice of prosthesis depends on the condition of the joint surfaces and on the anatomy and functional condition of the rotator cuff.
- The damaged humeral head is removed, or is sometimes just resurfaced. In this case, a ‘cap’ is placed over the humeral head and not all of the bone is removed.
- The component that replaces the head of the humerus is made of an alloy based on cobalt and chromium. It comes in various sizes and can be a single piece or a modular unit.
- The component that replaces the glenoid depression is made of ultra-high-density polyethylene. Some varieties have a metal tray but totally plastic versions are more common.
- The surgeon may replace just the humeral head in a hemiarthroplasty, or both the
 humeral head and the glenoid in a total shoulder replacement.
humeral head and the glenoid in a total shoulder replacement. - The use of bone cement is dictated by the quality of the patient’s bone stock but is routinely used when a fracture is being treated.[9]
- The glenoid component is held in place by either acrylic bone cement (cemented) or bone in growth (cementless).
- The surrounding muscles and tendons provide stability for the prosthesis as with the normal shoulder.
- Several conditions can cause shoulder pain and disability, and lead patients to consider shoulder joint replacement surgery.
CAUSES
Osteoarthritis (Degenerative Joint Disease)
This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older, but may occur in younger people, too. The cartilage that cushions the bones of the shoulder softens and wears away. The bones then rub against one another. Over time, the shoulder joint slowly becomes stiff and painful.
Unfortunately, there is no way to prevent the development of osteoarthritis. It is a common reason people have shoulder replacement surgery.
Osteoarthritis of the shoulder.
Rheumatoid Arthritis
This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed “inflammatory arthritis.”
Post-traumatic Arthritis
This can follow a serious shoulder injury. Fractures of the bones that make up the shoulder or tears of the shoulder tendons or ligaments may damage the articular cartilage over time. This causes shoulder pain and limits shoulder function.
Rotator Cuff Tear Arthropathy
A patient with a very large, long-standing rotator cuff tear may develop cuff tear arthropathy. In this condition, the changes in the shoulder joint due to the rotator cuff tear may lead to arthritis and destruction of the joint cartilage.
Avascular Necrosis (Osteonecrosis)
Avascular necrosis is a painful condition that occurs when the blood supply to the bone is disrupted. Because bone cells die without a blood supply, osteonecrosis can ultimately cause destruction of the shoulder joint and lead to arthritis. Chronic steroid use, deep sea diving, severe fracture of the shoulder, sickle cell disease, and heavy alcohol use are risk factors for avascular necrosis.
Severe Fractures
A severe fracture of the shoulder is another common reason people have shoulder replacements. When the head of the upper arm bone is shattered, it may be very difficult for a doctor to put the pieces of bone back in place. In addition, the blood supply to the bone pieces can be interrupted. In this case, a surgeon may recommend a shoulder replacement. Older patients with osteoporosis are most at risk for severe shoulder fractures.
Failed Previous Shoulder Replacement Surgery
Although uncommon, some shoulder replacements fail, most often because of implant loosening, wear, infection, and dislocation. When this occurs, a second joint replacement surgery — called a revision surgery — may be necessary.
Is Shoulder Joint Replacement for You?
The decision to have shoulder replacement surgery should be a cooperative one between you, your family, your family physician, and your orthopaedic surgeon.
There are several reasons why your doctor may recommend shoulder replacement surgery. People who benefit from surgery often have:
- Severe shoulder pain that interferes with everyday activities, such as reaching into a cabinet, dressing, toileting, and washing.
- Moderate to severe pain while resting. This pain may be severe enough to prevent a good night’s sleep.
- Loss of motion and/or weakness in the shoulder.
- Failure to substantially improve with other treatments such as anti-inflammatory medications, cortisone injections, or physical therapy.
Postoperative care and rehabilitation
A well-planned rehabilitation programme is essential for success.
Therapy should begin very soon after surgery. A physiotherapist will start gentle, passive and active assisted range of movement exercises. The safe range of movement will depend on the type of surgical approach. In the deltopectoral approach, the subscapularis tendon is either surgically divided or elevated with a lesser tuberosity osteotomy. Range of movement allowed will depend on the adequacy of fixation.
Hospital stay varies from two to five days and is dependent on patient comorbidities.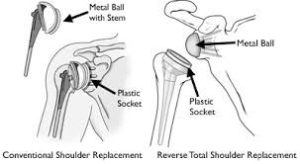
Advice following discharge usually includes:
- Wear the sling every night for at least the first month.
- Do not use the arm to push up in bed or from a chair.
- Follow the exercise programme diligently.
- Do not overdo it. Early overuse of the shoulder may result in restricted movement later.
- Do not lift anything heavier than a cup of tea or coffee for the first six weeks after surgery.
- Do not do any contact sports or heavy lifting for at least six month
Complications
Your orthopaedic surgeon will explain the potential risks and complications of shoulder joint replacement, including those related to the surgery itself and those that can occur over time after your surgery.
When complications occur, most are successfully treatable. Possible complications include the following.
Infection
Infection is a complication of any surgery. In shoulder joint replacement, infection may occur in the wound or deep around the prosthesis. It may happen while in the hospital or after you go home. It may even occur years later. Minor infections in the wound area are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis.
Any infection in your body can spread to your joint replacement.
Prosthesis Problems
Although prosthesis designs and materials, as well as surgical techniques, continue to advance, the prosthesis may wear down and the components may loosen. The components of a shoulder replacement may also dislocate. Excessive wear, loosening, or dislocation may require additional surgery (revision procedure).
Nerve Injury
Nerves in the vicinity of the joint replacement may be damaged during surgery, although this type of injury is infrequent. Over time, these nerve injuries often improve and may completely recover.
Do’s and Don’ts
The success of your surgery will depend largely on how well you follow your orthopaedic surgeons instructions at home during the first few weeks after surgery. Here are some common do’s and don’ts for when you return home:
- Don’t use the arm to push yourself up in bed or from a chair because this requires forceful contraction of muscles.
- Do follow the program of home exercises prescribed for you. You may need to do the exercises 2 to 3 times a day for a month or more.
- Don’t overdo it! If your shoulder pain was severe before the surgery, the experience of pain-free motion may lull you into thinking that you can
- Do more than is prescribed. Early overuse of the shoulder may result in severe limitations in motion.
- Don’t lift anything heavier than a glass of water for the first 2 to 4 weeks after surgery.
- Do ask for assistance. Your physician may be able to recommend an agency or facility if you do not have home support.
- Don’t participate in contact sports or do any repetitive heavy lifting after your shoulder replacement.
- Do avoid placing your arm in any extreme position, such as straight out to the side or behind your body for the first 6 weeks after surgery.
- Many thousands of patients have experienced an improved quality of life after shoulder joint replacement surgery. They experience less pain, improved motion and strength, and better function.
