 Overview on retinal replacement:
Overview on retinal replacement:
It’s important to act quickly if you have symptoms of a retinal detachment. Retinal detachment surgery can restore circulation to the retina and preserve vision. Minor surgeries can be performed in your doctor’s office. More serious surgeries require a trip to the hospital.
A retinal detachment is a separation of the retina from its attachments to the underlying tissue within the eye. A retinal detachment almost always affects only one eye at a time. The second eye, however, must be checked thoroughly for any signs of predisposing factors.
Most retinal detachments are a result of a retinal break, hole, or tear. Most retinal breaks, holes, or tears are not the result of trauma but are due to preexisting factors such as high levels of myopia, prior ocular surgery, and other eye diseases.
Flashing lights and floaters may be the initial symptoms of a retinal detachment or of a retinal tear that precedes the detachment itself.
Early diagnosis and repair of retinal detachments are important since visual improvement is much greater when the retina is repaired before the macula or central area is detached.
The surgical repair of a retinal detachment is usually successful in reattaching the retina.
Retinal detachment is a serious condition of the eye in which the retina sto ps receiving oxygen. The symptoms of a retinal detachment can be frightening. Objects might appear to float across your eye, or a gray veil may move across your field of vision. If not treated quickly, a retinal detachment can cause you to lose your vision. Retinal detachment repair is a surgery that is used to restore circulation to the retina and preserve vision. If you have the symptoms described above, you should call your ophthalmologist or go to the emergency department immediately.
ps receiving oxygen. The symptoms of a retinal detachment can be frightening. Objects might appear to float across your eye, or a gray veil may move across your field of vision. If not treated quickly, a retinal detachment can cause you to lose your vision. Retinal detachment repair is a surgery that is used to restore circulation to the retina and preserve vision. If you have the symptoms described above, you should call your ophthalmologist or go to the emergency department immediately.
Why is a retinal detachment repair performed?
Your retina is the part of your eye that sends images through your optic nerve to the brain. Your retina contains millions of cells that detect light like a camera. It is part of the very back of your eyeball and is essential to your vision.
Retinal detachment occurs when the retina pulls away from the back of the eye and the blood supply. Without a blood supply, the retinal cells will start to die. This can cause permanent damage to your vision. If the macula (central vision area) begins to loosen, your vision may be permanently damaged. If the macula completely detaches, you may lose your vision entirely. Reattaching the retina quickly is essential to prevent such a serious complication.
Retinal detachment can occur because the vitreous fluid of the eye (a gel-like liquid) retracts from the back of the eye, pulling the retina and tearing it. That tear can then pull away from the back of the eye and detach the retina. Some causes and risk factors of retinal detachment include glaucoma, severe trauma, nearsightedness, previous cataract surgery, previous retinal detachment in your other eye, or family history of retinal detachment.
How is a retinal detachment repair performed?
There are several types of surgery to repair a detached retina. A simple tear in the retina can be treated with freezing, called cryotherapy, or a laser procedure. Different types of retinal detachment require different kinds of surgery and different levels of anesthesia. The type of procedure your doctor preforms will depend on the severity of retinal detachment.
One method of retinal detachment repair is pneumatic retinopexy. In this procedure, a gas bubble is injected into the eye. The bubble presses against the detached retina and pushes it back into place. A laser or cryotherapy is then used to reattach the retina firmly into place. The gas bubble will dissolve in a few days. A pneumatic retinopexy can be done in an ophthalmologist’s office.
In more severe tears, a procedure called a scleral buckle may be performed. During a scleral buckle a doctor will place a flexible band around the eye to counteract the force that is pulling the retina out of place. The fluid behind the detached retina will be drained, and the retina should return to its normal place in the back of the eye.
This procedure is done in a hospital, operating room, or surgery clinic. Local or general anesthesia will be used, and you may need to stay overnight in the hospital.
A vitrectomy is a procedure done for serious retinal detachment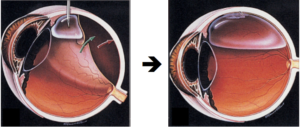 s. It may require partially removing the vitreous fluid inside the eye. Local anesthesia is used and the procedure is usually done in a surgical clinic.
s. It may require partially removing the vitreous fluid inside the eye. Local anesthesia is used and the procedure is usually done in a surgical clinic.
Surgery for retinal detachment
Surgery is the only treatment for retinal detachment camera.gif. The goals of surgery are:
- To reattach the retina.
- To prevent or reverse vision loss.
Almost all retinal detachments can be repaired with scleral buckle surgery, pneumatic retinopexy, or vitrectomy.
But even with such a high rate of success for surgery, it is important to act quickly. The longer you wait to have surgery, the lower the chances that good vision will be restored. When the retina loses contact with its supporting layers, vision begins to get worse. An eye doctor (ophthalmologist) who specializes in retinal detachments will usually do surgery within a few days of your being diagnosed with a detachment.
How soon you need surgery usually depends on whether the retinal detachment has or could spread far enough to affect central vision. When the macula, the part of the retina that provides central vision, loses contact with the layer beneath it, it quickly loses its ability to process what the eye sees.
Having surgery while the macula is still attached will usually save vision.
If the macula has become detached, surgery may occur a few days later than it would have otherwise. Good vision after surgery is still possible but less likely.
Your doctor will decide how soon you need surgery based on the result of the retinal exam and the doctor’s experience in treating retinal detachment.
Surgery choices
Common methods of repairing a retinal detachment include:
Pneumatic retinopexy: In this procedure, your eye doctor injects a gas bubble into the middle of the eyeball. The gas bubble floats to the detached area and lightly presses the detached retina to the wall of the eye. The eye doctor then uses a freezing probe (cryopexy) or laser beam (photocoagulation) to seal the tear in the retina.
Scleral buckling surgery: Your eye doctor places a piece of silicone sponge, rubber, or semi-hard plastic on the outer layer of your eye and sews it in place. This relieves pulling (traction) on the retina, preventing tears from getting worse, and it supports the layers of the retina.
Vitrectomy: This is the removal of the vitreous gel from the eye. Vitrectomy gives your eye doctor better access to the retina and other tissues. It allows him or her to peel scar tissue off the retina, repair holes, close very large tears, and directly flatten a retinal detachment.
What to think about before the surgery?
You have several surgical options to repair a retinal detachment. Their success in restoring good vision varies from case to case. The cause, location, and type of detachment usually determine which surgery will work best. Other conditions or eye problems may also play a role when you choose the best type of surgery.
You may need more than one surgery to reattach the retina if scar tissue from the first surgery grows over the surface of your retina.
Things that may make surgery more difficult include:
- Pupils that will not get larger (dilate).
- Infection inside or outside the eye.
- Scarring from previous surgery.
- Bleeding (hemorrhage) in the vitreous gel.
- Scars on or cloudiness in the cornea.
- Clouding of the lens (cataract).
After surgery, you may need to use antibiotic eyedrops and corticosteroid medicines for a short time.
What are the risks of retinal detachment repair?
Surgery always carries some risk. If you have general anesthesia, it can interfere with breathing. Some people have serious reactions to the medication.
If the retina was damaged before reattachment, there can be permanent loss of vision.
Risks Of Retinal Repair Surgery
The specific risks of retinal repair surgery include as follows:
- infection
- bleeding in the eye
- high pressure inside the eye (glaucoma)
- cataract (clouding of the lens)
- the need for additional surgeries
What can be expected in the long term?
Usually the retina can be attached in a single operation, but sometimes multiple procedures are required. More than 90 percent of detachments can be repaired. In the less than 10 percent of detachments that cannot be repaired, the patient will have either poor vision or no vision in that eye.
The success of a retinal repair depends on the seriousness of the tears and detachment and how much scar tissue was formed in the retina. If the macula or central portion of the retina was not affected, vision will be good. If the macula was detached for a long time, some vision will return, but it will often be less than 20/200, which is legally blind. It may take several months of healing after surgery to determine how much vision will return.
