What is Laryngectomy?
It is the surgical removal of the larynx. The larynx is the portion of your throat that houses your vocal cords, which allow you to produce sound. The larynx connects your nose and mouth to your lungs. It also protects your breathing system by keeping the things you eat or drink in your oesophagus and out of your lungs.
If you have a laryngectomy, it will affect your speaking, swallowing, and breathing. You’ll need to learn new ways to perform all three tasks after surgery.
The larynx is composed of cartilage and divided into three main sections: the supraglottis, the glottis, and the sub glottis. When a patient undergoes a laryngectomy, the trachea (windpipe) and the oesophagus (food pipe) are disconnected and thus breathing and swallowing will be different after surgery. In order to breathe, a stoma (hole) is placed in the neck, in front of the trachea. Speech may be regained in certain cases, when a transesophageal puncture (TEP), a hole in both the trachea and oesophagus, is placed for future prosthetic voice box placement.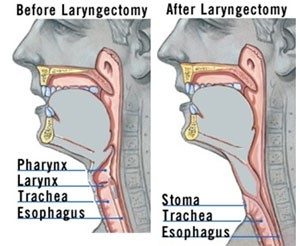
A laryngectomy may be recommended in cases of certain medical conditions including laryngeal cancer. It may also be recommended in non-cancerous or benign conditions like an injury or radiation necrosis secondary from prior radiation treatment. The person who has the laryngectomy is called a larengectomee.
Why it is to be done?
Because of its location, the voice box, or larynx, plays a critical role in breathing, swallowing, and speaking. The larynx is located above the windpipe (trachea) and in front of the food pipe (oesophagus). It contains two small bands of muscle called the vocal cords that close to prevent food from entering the lungs and vibrate to produce the voice. If cancer of the larynx develops, a laryngectomy is performed to remove tumours or cancerous tissue. In rare cases, the procedure may also be performed when the larynx is badly damaged by gunshot, automobile injuries, or other traumatic accidents.
There are several different types of laryngectomy, including:
Total Laryngectomy: During a total laryngectomy, the whole larynx (voice box) is removed, at which time a permanent stoma is created to create a new way to breathe (tracheostomy). This procedure may require that a portion of the pharynx (the tubular structure connecting the nose, larynx and lungs), some lymph nodes, and some surrounding muscles also be removed. The surgeon may perform a transesophageal puncture (TEP), or put a hole in both the trachea and oesophagus, for future prosthetic voice box placement.
Partial Laryngectomy: During a partial laryngectomy, a portion of the larynx (voice box) is removed. This option is dependent on where the cancer or abnormality is located. It may be necessary to have a temporary tracheostomy placed, which can be removed at a later time.
Removing part of the voice box (partial laryngectomy)
You might have a partial laryngectomy for early laryngeal cancer, or cancer that has come back after treatment (recurrent cancer).
How you have it 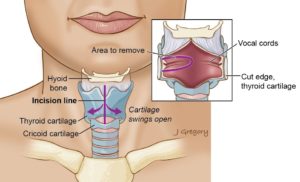
The surgeon makes a cut in your neck. They remove part of your voice box (larynx). This is called an open partial laryngectomy. Surgery through your mouth (endoscopic surgery) is becoming a more common surgery to remove part of your voice box (larynx).
You keep at least part of one vocal cord. You are usually still able to speak afterwards. But your voice may be quite hoarse or weak.
During the operation the surgeon also makes a hole in your neck, which you breathe through. The hole is called a stoma (tracheostomy). The tracheostomy allows your voice box to heal after the surgery.
Most people who have a partial laryngectomy have a temporary tracheostomy. After a brief recovery time, your nurse removes your tracheostomy tube and your stoma gradually closes up. Once it has closed, you can start to speak naturally again. Some people need a permanent tracheostomy, but this is rare.
Removing the voice box (total laryngectomy)
Your surgeon might remove the whole of your voice box (larynx) to remove your cancer. This is called a total laryngectomy. Part of the pharynx might also be removed.
Your larynx is the connection between your mouth and your lungs. After it is removed, that connection is no longer there.
So your surgeon attaches the end of your windpipe to a hole in your neck, which you now breathe through. This is called a stoma. After a total laryngectomy, this stoma is permanent. You will now always breathe through your stoma.
Preparing for surgery
Your doctor and care team will let you know what you need to do to prepare for surgery. In general, you should not eat or drink anything (except essential medications) anytime after midnight prior to surgery. You should inform your doctor if you have a fever, productive cough or any other signs of infection. Your doctor will give you a medical clearance evaluation and give recommendations to optimize all the other organs in your body prior to undergoing general anaesthesia and surgery.
On the day of surgery, you will need to arrive at the hospital or surgery centre a few hours before the scheduled operation. This allows the nurses and anaesthesiologist to confirm everything is in order for you to have as safe a surgery as possible. You will see your surgeon one last time before receiving the anaesthesia and falling asleep, and you can ask any last-minute questions at that time.
If you are undergoing a laryngectomy, you should have had a discussion with a speech and swallow therapist prior to surgery.
Laryngectomy Procedure
The surgeon begins the procedure by making incisions in your neck through which he or she will remove your larynx. Lymph nodes and part of your pharynx may also be removed, depending on the underlying cause of your laryngectomy. Lymph nodes are part of your immune system and located throughout your body. They help fight infection, but they can also be affected by cancer.
Your pharynx is the common space in the back of your throat where you’re nasal passages, mouth, upper oesophagus, and your larynx all meet. Treatment for cancer of your pharynx might involve partial removal of your pharynx. This is called a pharyngectomy.
After removing the larynx, the doctor will create the stoma, a permanent hole about the size of a nickel in the front of the trachea. It links directly from the outside to your lungs so you can breathe.
Some people who have laryngectomy also have a tracheoesophageal pun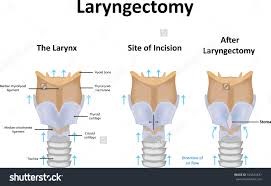 cture (TEP) performed. By going through the stoma, a small hole is created in both the trachea and the oesophagus. This can be done at the time as the laryngectomy surgery or during a second procedure afterwards. Something must always remain in place within the TEP in order to keep it open.
cture (TEP) performed. By going through the stoma, a small hole is created in both the trachea and the oesophagus. This can be done at the time as the laryngectomy surgery or during a second procedure afterwards. Something must always remain in place within the TEP in order to keep it open.
Once the surgery is complete, your throat muscles and the skin on your neck will be closed with surgical stitches. You might have drainage tubes placed in your neck before you’re taken to the recovery room. The tubes drain the surgical site of fluids and blood for several days after a laryngectomy.
Aftercare
A person undergoing a laryngectomy spends several days in intensive care (ICU) and receives intravenous (IV) fluids and medication. As with any major surgery, blood pressure, pulse, and respiration are monitored regularly. The patient is encouraged to turn, cough, and deep-breathe to help mobilize secretions in the lungs. One or more drains are usually inserted in the neck to remove any fluids that collect. These drains are removed after several days.
It takes two to three weeks for the tissues of the throat to heal. During this time, the laryngectomy cannot swallow food and must receive nutrition through a tube inserted through the nose and down the throat into the stomach. Normal speech is also no longer possible and patients are instructed in alternate means of vocal communication by a speech pathologist.
When air is drawn in normally through the nose, it is warmed and moistened before it reaches the lungs. When air is drawn in through the stoma, it does not have the opportunity to be warmed and humidified. In order to keep the stoma from drying out and becoming crusty, laryngectomees are encouraged to breathe artificially humidified air. The stoma is usually covered with a light cloth to keep it clean and to keep unwanted particles from accidentally entering the lungs. Care of the stoma is extremely important, since it is the person’s only way to get air to the lungs. After a laryngectomy, a health-care professional will teach the laryngectomy and his or her caregivers how to care for the stoma.
There are three main methods of vocalizing after a total laryngectomy. In oesophageal speech, patients learn how to “swallow” air down into the oesophagus and create sounds by releasing the air. Tracheoesophageal speech diverts air through a hole in the trachea made by the surgeon. The air then passes through an implanted artificial voice. The third method involves using a hand-held electronic device that translates vibrations into sounds. The choice of vocalization method depends on several factors including the age and health of the laryngectomy, and whether other parts of the mouth, such as the tongue, have also been removed.
Risks May Include:
- Complications associated with anaesthesia
- Medication reactions
- Bleeding
- Blood clots
- Infection
- Pneumonia
- Heart or lung problems
- Loss of normal speech
- Nerve injury
- Excessive swelling
- Throat or larynx narrowing, known as stenosis, which may require placement of a tracheostomy of the stoma, known as stomal stenosis
- Difficulty swallowing, at times requiring a permanent feeding tube
- Development of a fistula (abnormal connection between the pharynx and the skin) which may require corrective surgery
- Carotid artery rupture (rare, yet very serious)
- Damage to surrounding organs likes the thyroid and parathyroid glands; this can lead to hypothyroidism and/or calcium abnormalities. Other organs that can be damaged are the trachea and oesophagus
- Hematoma (collection of blood)
- Leaking around the newly placed TEP/prosthesis
How Can I Care for Myself?
Depending on the extent of your surgery, you may need a family member or friend to help you with your daily tasks until you are feeling better and your medical team gives you the go ahead to resume normal activity.
Be sure to take your medications as directed to prevent pain, infection and/or constipation and call your medical team with any concerning symptoms.
Deep breathing and relaxation are important to help with pain, keep lungs healthy after anaesthesia, and promote good drainage of lymphatic fluid. Try to perform deep breathing and relaxation exercises several times a day in the first week, or whenever you notice you are particularly tense.
Speaking after a laryngectomy
Without your vocal cords and with a stoma, you are not able to speak in the normal way. This can be very difficult to cope with. But there are now several ways to help you make sounds and learn to speak again.
A speech therapist visits you before your operation to discuss the different ways of communicating after surgery.
Stoma care
Learning to care for your stoma is an essential part of the recovery process after a laryngectomy. The stoma opening can introduce bacteria and viruses into your body that can lead to infection. Proper care can limit this type of complication.
You’ll want to clean the edges of the stoma with gauze and mild soap and water. Gently remove crusting and excess mucus. Salt water spray can help with this. Crusting can impede the airflow to your lungs. Your healthcare provider should provide you with detailed instructions, as well as information on what to do in case of emergencies.
Coughing can help clear your stoma of mucus. If you’re not strong enough to cough forcefully, you may need to manually suction out the stoma. Your healthcare provider can show you how to suction properly so as not to cause infection.
Humid air helps prevent crusting of the stoma. Use a humidifier in your home, especially in your bedroom at night. Your doctor might recommend you use a special mask that delivers humidified air directly to your stoma for a period of time. This is more common when a stoma is new. Once the skin around your stoma “matures,” or becomes used to the dry air, you’ll no longer need the mask.
