 Overview on deep brain stimulation:
Overview on deep brain stimulation:
Deep brain stimulation involves implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that regulate abnormal impulses. Or, the electrical impulses can affect certain cells and chemicals within the brain.
Deep brain stimulation is used to treat a number of neurological conditions, such as:
- Essential tremor
- Parkinson’s disease
- Dystonia
- Epilepsy
- Tourette syndrome
- Chronic pain
- Obsessive compulsive disorder
Deep brain stimulation (DBS) is a surgery to implant a device that sends electrical signals to brain areas responsible for body movement. Electrodes are placed deep in the brain and are connected to a stimulator device. Similar to a heart pacemaker, a neurostimulator uses electric pulses to regulate brain activity. DBS can help reduce the symptoms of tremor, slowness of movement, stiffness, and walking problems caused by Parkinson’s disease, dystonia, or essential tremor. Successful DBS allows people to better manage their symptoms, reduce their medications, and improve their quality of life.
What is deep brain stimulation?
In deep brain stimulation, electrodes are placed in a specific area of the brain (usually the subthalamic nucleus) depending on the symptoms being treated. The electrodes are placed on both the left and right sides of the brain through small holes made at the top of the skull. The electrodes are connected by long extension wires that are passed under the skin and down the neck to a battery-powered stimulator under the skin of the chest. When turned on, the stimulator sends electrical pulses to block the faulty nerve signals causing tremors, rigidity, and other symptoms.
A deep brain stimulator system has three parts that are implanted inside the body:
Neurostimulator – a programmable battery-powered pacemaker device that creates electric pulses. It is placed under the skin of the chest below the collarbone or in the abdomen.
Lead – a coated wire with a number of electrodes at the tip that deliver electric pulses to the brain tissue. It is placed inside the brain and connects to an extension wire through a small hole in the skull.
Extension – an insulated wire that connects the lead to the neurostimulator. It is placed under the skin and runs from scalp, behind the ear, down the neck, and to the chest.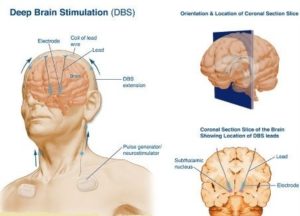
The patient uses a handheld controller to turn the DBS system on and off. The doctor programs the stimulator settings with a wireless device. The stimulation settings can be adjusted as a patient’s condition changes over time. Unlike other surgeries, such as pallidotomy or thalamotomy, DBS does not damage the brain tissue. Thus, if better treatments develop in the future, the DBS procedure can be reversed.
DBS is very effective at reducing dyskinesias, the uncontrolled wiggling movements caused by high doses of levadopa medication.
Why it is done?
Deep brain stimulation is an established treatment for movement disorders, such as essential tremor, Parkinson’s disease and dystonia, and more recently, obsessive-compulsive disorder.
Who is a candidate?
You may be a candidate for DBS if you have:
- A movement disorder with debilitating symptoms (tremor, stiffness) and your medications have begun to lose effectiveness.
- Troubling “off” periods when your medication wears off before the next dose can be taken.
- Troubling “on” periods when you develop medication-induced dyskinesias (excessive wiggling of the torso, head, and/or limbs).
- DBS may not be an option if you have severe untreated depression, advanced dementia, or if you have symptoms that are not typical for Parkinson’s disease.
DBS can help treat many of the symptoms caused by the following movement disorders:
Parkinson’s disease: tremor, rigidity, and slowness of movement caused by the death of dopamine-producing nerve cells responsible for relaying messages that control body movement.
Essential tremor: involuntary rhythmic tremors of the hands and arms, occurring both at rest and during purposeful movement. Also may affect the head in a “no-no” motion.
Dystonia: involuntary movements and prolonged muscle contraction, resulting in twisting or writhing body motions, tremor, and abnormal posture. May involve the entire body, or only an isolated area. Spasms can often be suppressed by “sensory tricks,” such as touching the face, eyebrows, or hands.
A team of specialists including a neurologist, neuropsychologist, and neurosurgeon will evaluate your condition to determine if surgery is an option. Your thinking and memory, current medications, and general health will be evaluated. You will be videotaped performing a variety of movements (walking, finger tap, rising from a chair) while on and off medication. Your symptoms and abilities are measured using the Unified Parkinson Disease Rating Scale (UPDRS).
After your evaluation and videotaping is complete, your case will be discussed at a monthly conference with multiple physicians, nurses, and surgeons. The team discusses the best treatment plan for each patient. If the team agrees that you are a good candidate for DBS, you will be contacted to schedule an appointment with a neurosurgeon.
What happens before surgery?
You will typically undergo tests (e.g., blood test, electrocardiogram, chest X-ray) several days before surgery. An MRI scan of your brain will be performed. In the doctor’s office you will sign consent forms and complete paperwork to inform the surgeon about your medical history, including allergies, medicines, anaesthesia reactions, and previous surgeries.
Stop taking all non-steroidal anti-inflammatory medicines (Naprosyn, Advil, Motrin, Nuprin, Aleve, etc.) 1 week before surgery. Stop smoking, chewing tobacco, and drinking alcohol 1 week before and 2 weeks after surgery because these activities can cause bleeding problems. You may also need to have clearance from your primary care physician or cardiologist if you have a history of other medical or heart conditions. No food or drink, including your Parkinson’s medication, is permitted after midnight the night before surgery.
What happens before surgery?
You will typically undergo tests (e.g., blood test, electrocardiogram, chest X-ray) several days before surgery. An MRI scan of your brain will be performed. In the doctor’s office you will sign consent forms and complete paperwork to inform the surgeon about your medical history, including allergies, medicines, anesthesia reactions, and previous surgeries.
Try to get a good night’s sleep. The DBS surgery involves multiple steps and lasts most of the day, during which you will be awake and off medication.
What happens after surgery?
After surgery, you may take your regular dose of Parkinson’s medication immediately. You are kept overnight for monitoring and observation. Most patients are discharged home the next day.
During the recovery time after implanting the electrodes, you may feel better than normal. Brain swelling around the electrode tip causes a lesion effect that lasts a couple days to weeks. This temporary effect is a good predictor of your outcome once the stimulator is implanted and programmed.
About a week later, you will return to the hospital for outpatient surgery to implant the stimulator in the chest/abdomen. This surgery is performed under general anesthesia and takes about an hour. Patients go home the same day.
You will be taken to the OR and put to sleep with general anesthesia. A portion of the scalp incision is reopened to access the leads. A small incision is made near the collarbone and the neurostimulator is implanted under the skin. The lead is attached to an extension wire that is passed under the skin of the scalp, down the neck, to the stimulator/battery in the chest or abdomen. The device will be visible as a small bulge under the skin, but it is usually not seen under clothes.
You should avoid arm movements over your shoulder and excessive stretching of your neck while the incisions heal. Pain at the incision sites can be managed with medication.
About 10 days after surgery, you will be scheduled for an office visit. The stimulator will be programmed and your medication dosage will be adjusted. You may be asked to stop taking your medications for up to 12 hours before the programming session. This is done to increase the effectiveness of the programming in reducing your usual symptoms. It is important that you work with the neurologist and nurse to adjust your medications and refine the programming. You will return to the office every 3 weeks for programming. It typically takes 3 to 4 programming sessions to attain maximum symptom control while minimizing side effects.
Most people don’t feel the stimulation as it reduces their symptoms. However, some people may feel a brief tingling sensation when the stimulator is first turned on.
It’s important to remember that Parkinson’s disease is progressive and symptoms get worse over time. You will return to the neurologist’s office periodically to adjust the stimulation settings.
Surgery risks
Deep brain stimulation involves creating small holes in the skull to implant the electrodes. Complications of surgery may include:
- Bleeding in the brain
- Stroke
- Infection
- Breathing problems
- Nausea
- Heart problems
- Seizures
- Balance problems
- Lightheadedness
- Unwanted mood changes, such as mania and depression
What are the results?
Successful DBS is related to
1) Appropriate patient selection,
2) Appropriate selection of the brain area for stimulation,
3) Precise positioning of the electrode during surgery, and
4) experienced programming and medication management.
For essential tremor, DBS of the thalamus may significantly reduce hand tremor in 60 to 90% of patients and may improve head and voice tremor.
