Tympanoplasty:
Tympanoplasty is also called as eardrum repair, refers to surgery performed to reconstruct a perforated tympanic membrane (eardrum) or the small bones of the middle ear. Eardrum perforation may result from chronic infection or, less commonly, from trauma to the eardrum.
The eardrum is a thin membrane between your outer ear and your middle ear that vibrates when sound waves hit it. Repeated ear infections, surgery, or trauma may cause damage to your eardrum or middle ear bones that must be corrected with surgery. Damage to the eardrum or middle ear bones can result in hearing loss and an increased risk of ear infections.
Tympanoplasty is a safe and effective outpatient procedure used to both eradicate disease from the middle ear and restore hearing and middle ear function.
Why Tympanoplasty?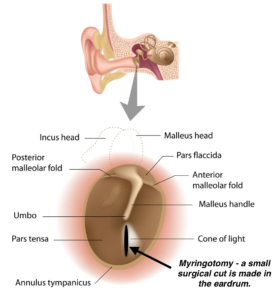
The tympanic membrane of the ear is a three-layer structure. The outer and inner layers consist of epithelium cells. Perforations occur as a result of defects in the middle layer and hearing loss, which contains elastic collagen fibers. Small perforations usually heal spontaneously. However, if the defect is relatively large, or if there is poor blood supply or an infection during the healing process, spontaneous repair may be hindered. Eardrums may also be perforated as a result of trauma, such as an object in the ear, a slap on the ear, or even an explosion.
The purpose of tympanoplasty is to repair the perforated eardrum, and sometimes the middle ear bones (ossicles) that consist of the incus, malleus, and stapes. Tympanic membrane grafting may be required. If needed, grafts are usually taken from a vein or fascia (muscle sheath) tissue on the lobe of the ear. Synthetic materials may be used if patients have had previous surgeries and have limited graft availability.
What is Tympanoplasty?
A tympanoplasty is performed if the hole in your eardrum is large or if you have a chronic ear infection that cannot be cured with antibiotics or any other option. You will most likely be in the hospital for this surgery and will be placed under general anesthesia. You will be unconscious during this procedure.
First, the surgeon will use a laser to carefully remove any excess tissue or scar tissue that has built up in your middle ear. Then, a small piece of your own tissue will be taken from a vein or muscle sheath and grafted onto your eardrum to close the hole. The surgeon will either go through your ear canal to repair the eardrum or make a small incision behind your ear or access your eardrum that way. This procedure typically takes two to three hours.
Post-operative care: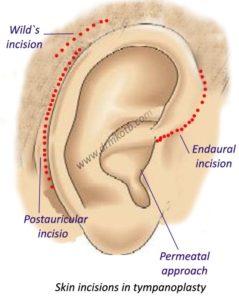
It is designed to keep the patient comfortable. Infection is 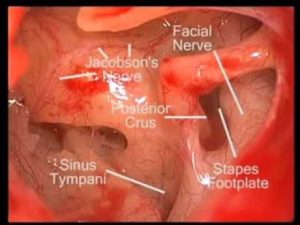 generally prevented by soaking the ear canal with antibiotics. To heal, the graft must be kept free from infection, and must not experience shearing forces or excessive tension. Activities that change the tympanic pressure are forbidden, such as sneezing with the mouth shut, using a straw to drink, or heavy nose blowing. A complete hearing test is performed four to six weeks after the operation.
generally prevented by soaking the ear canal with antibiotics. To heal, the graft must be kept free from infection, and must not experience shearing forces or excessive tension. Activities that change the tympanic pressure are forbidden, such as sneezing with the mouth shut, using a straw to drink, or heavy nose blowing. A complete hearing test is performed four to six weeks after the operation.
The process in detail:
- Surgery to reconstruct the tympanic membrane (eardrum) can be performed either under local or general anesthesia. An incision is made into the ear canal and the remaining eardrum is elevated away from the bony ear canal and lifted forward.
- The ear is perforated with a large hole. This gains access to the perforation. Once the hole is exposed fully, the perforated remnant is rotated forward, and the bones of hearing are inspected. There may be scar tissue and bands surrounding the bones of hearing. These can be removed either with micro hooks or laser.
3.After identifying the bones of hearing, the ossicular chain is pressed to determine if the chain is mobile and functioning. If the chain is mobile, then the remaining surgery concentrates on repairing the drum defect.
- Now, the tissue is taken either from the back of the ear or from the small cartilaginous lobe of skin in front the ear called the tragus. These tissues are thinned and dried. An absorbable gelatin sponge is placed under the drum to allow for support of the graft. The graft is then inserted underneath the remaining drum remnant and the drum remnant is folded back onto the perforation to provide closure.
- Very thin plastic sheeting is generally placed against the top of the graft to prevent it from sliding out of the ear when the patient blows his nose or sneezes. A small amount of Gelfoam is also placed on the outside of the silastic to hold it into position in a so-called sandwich type layer (drawing).
- If opened from behind, the ear is then stitched together. Usually, the stitches are buried in the skin and do not have to be removed later.
Types of tympanoplasty procedures:
- Type I tympanoplasty is called myringoplasty, and only involves the restoration of the perforated eardrum by grafting.
- Type II tympanoplasty is used for tympanic membrane perforations with the erosion of the malleus. It involves grafting onto the incus or the remains of the malleus.
- Type III tympanoplasty is indicated for the destruction of two ossicles, with the stapes still intact and mobile. It involves placing a graft onto the stapes and providing protection for the assembly.
- Type IV tympanoplasty is used for ossicular destruction, which includes all or part of the stapes arch. It involves placing a graft onto or around a mobile stapes footplate.
- Type V tympanoplasty is used when the footplate of the stapes is fixed.
Depending on its type, tympanoplasty can be performed under local or general anaesthesia. In small perforations of the eardrum, Type I tympanoplasty can be easily performed under local anaesthesia with intravenous sedation. An incision is made into the ear canal and the remaining eardrum is elevated away from the bony ear canal, and lifted forward.
The surgeon uses an operating microscope to enlarge the view of the ear structures. If the perforation is very large or the hole is far forward and away from the view of the surgeon, it may be necessary to perform an incision behind the ear. This elevates the entire outer ear forward, providing access to the perforation. Once the hole is fully exposed, the perforated remnant is rotated forward, and the bones of hearing are inspected. If scar tissue is present, it is removed either with micro hooks or laser.
Failure chances:
Failure of tympanoplasty can occur either from an immediate infection during the healing period, from water getting into the ear, or from the displacement of the graft after surgery. Most patients can expect a full “take” of the grafted eardrum and improvement in hearing.
After three to four months, water can be allowed to enter the ear and the patient can even return to swimming and other activities.
A total hearing loss from tympanoplasty surgery is very rare. This occurs in less than one percent of operations. Postoperative dizziness and imbalance can be present for about a week after surgery and are usually very mild.
If the ear becomes infected postoperatively, the risk of dizziness increases. Generally, all imbalance and dizziness will be resolved after a week or two.
Tinnitus or noises in the ear, particularly an echo-type feeling, may be present as a result of the perforation itself. Usually, with improvement in hearing and closure of the eardrum, these sensations clear up. However, tinnitus is unpredictable.
A small nerve goes through the ear called as the chorda tympany nerve. This nerve goes to the taste buds of the tongue. If this nerve is stretched or cut during tympanoplasty surgery, there may be a transient period of one or two months after surgery where there is a slightly metallic or salty taste to food. Generally, the nerve connections will regenerate and taste will return to normal. The abnormal taste sensation rarely lasts longer than six months and much.
After the procedure:
1.After about ten days, the packing is removed and a good evaluation can then be obtained as to whether the graft was successful.
- Water is kept away from the ear and blowing of the nose is discouraged. If there are allergies or a cold, further antibiotics and decongestant should be given.
3.Most individuals can return to work after five or six days unless they perform heavy physical labor, in which case the patient can return after two or three weeks.
- After three weeks, all packing is completely removed under the operating microscope in the office. It can then be determined whether the graft has fully taken.
5.In over 90 percent of the cases, the tympanoplasty procedure is successful and a hearing test is performed at four to six weeks after the operation.
Alternatives
Myringoplasty is another operative procedure used in the reconstruction of a perforation of the tympanic membrane. It is performed when the middle ear space, its mucosa, and the ossicular chain are free of active infection. Unlike tympanoplasty, there is no direct inspection of the middle ear during this procedure.
