Brief about Bariatric Surgery:-
Bariatric surgery is a safe and effective treatment option for those affected by severe obesity. Moreover, these same procedures have also been recognized for their impact on metabolic or hormonal changes that play a major role in hunger (the desire to start eating) and satiety (the desire to stop eating) as well as improvement and/or resolution of conditions that can occur as a result of severe obesity.
Bariatric surgery is a recognized and accepted approach for both weight-loss and many of the conditions that occur as a result of severe obesity; however, not all people affected by severe obesity will qualify for bariatric surgery. There are certain criteria that a person must meet in order to be a candidate for bariatric surgery.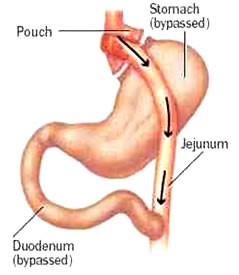
Today, there are also FDA-approved bariatric devices available for the treatment of obesity, such as intragastric balloons. These devices are not approved for the treatment of severe obesity.
Am I a Candidate for Weight Loss Surgery?
You may be a candidate for weight loss or obesity surgery if you have:
A body mass index (BMI) of 30 or more or about 100 pounds overweight for men and 80 pounds for women.
Benefits from Bariatric Surgery:-
Within two to three years after the operation, bariatric surgery usually results in a weight-loss of 10 to 35 percent of total body weight, depending on the chosen procedure. Those considering bariatric surgery should talk to their PCP about what their personal expectations should be for loss of excess weight. In addition, co-morbidities, such as diabetes, high blood pressure, sleep apnoea and others are often reduced or may go into remission. Most will find they require fewer medicines throughout time and many will discontinue their medicines completely.
Risks:-
Research indicates that some patients who undergo bariatric surgery may have unsatisfactory weight-loss or regain much of the weight that they lost. Some behaviours such as frequent snacking on high-calorie foods or lack of exercise can contribute to inadequate weight-loss. Technical problems that may occur after the operation, like separated stitches, may also contribute to inadequate weight-loss. There are also other potential complications that may occur which have been listed below with each of the various procedures.
Differentiate between open and laparoscopic surgery?
In open bariatric surgery, surgeons make a single, large cut in the abdomen. More often, surgeons now use laparoscopic surgery, in which they make several small cuts and insert thin surgical tools through the cuts. Surgeons also insert a small scope attached to a camera that projects images onto a video monitor. Laparoscopic surgery has fewer risks than open surgery and may cause less pain and scarring than open surgery. Laparoscopic surgery also may lead to a faster recovery.
Open surgery may be a better option for certain people. If you have a high level of obesity, have had stomach surgery before, or have other complex medical problems, you may need open surgery.
Throughout this section, you will see terms, such as “metabolic”, ““non-metabolic,” “laparoscopic” and “open,” in which you may not be familiar. Prior to reading about the different surgeries, we have provided you with a brief description of some of the most commonly used terms when talking about bariatric surgery.
Surgical Options:-
Surgeons use three types of operations most often:
- laparoscopic adjustable gastric band
- gastric sleeve surgery, also called sleeve gastrectomy
- gastric bypass
Surgeons use a fourth operation, biliopancreatic diversion with duodenal switch, less often.
Laparoscopic adjustable gastric band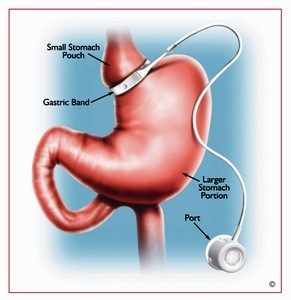
In this type of surgery, the surgeon places a ring with an inner inflatable band around the top of your stomach to create a small pouch. This makes you feel full after eating a small amount of food. The band has a circular balloon inside that is filled with salt solution. The surgeon can adjust the size of the opening from the pouch to the rest of your stomach by injecting or removing the solution through a small device called a port placed under your skin.
After surgery, you will need several follow-up visits to adjust the size of the band opening. If the band causes problems or is not helping you lose enough weight, the surgeon may remove it.
Weight-loss:
Weight-loss with an adjustable gastric band is typically slow and steady. Band patients generally lose one to two pounds per week during the first year after band placement. On average, by year one, band patients lost approximately 14 percent of their total body weight (weight at time of procedure). In a 350 pound person, this would mean a 49 pound weight-loss. By year three, band patients lost approximately 15.9 percent of their total body weight (weight at time of procedure).
Conclusion:
Adjustable gastric banding is an effective weight-loss operation that can lead to meaningful, long-term weight-loss. No matter what weight-loss operation is chosen, individuals need to change their lifestyle and learn to work with the surgery in order to be successful.
Gastric Sleeve
In gastric sleeve surgery, also called vertical sleeve gastrectomy, a surgeon removes most of your s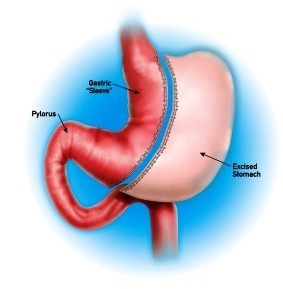 tomach, leaving only a banana-shaped section that is closed with staples. Like gastric band surgery, this surgery reduces the amount of food that can fit in your stomach, making you feel full sooner. Taking out part of your stomach may also affect gut hormones or other factors such as gut bacteria that may affect appetite and metabolism. This type of surgery cannot be reversed because some of the stomach is permanently removed.
tomach, leaving only a banana-shaped section that is closed with staples. Like gastric band surgery, this surgery reduces the amount of food that can fit in your stomach, making you feel full sooner. Taking out part of your stomach may also affect gut hormones or other factors such as gut bacteria that may affect appetite and metabolism. This type of surgery cannot be reversed because some of the stomach is permanently removed.
The majority of LSG’s performed today are completed laparoscopically. During the LSG, about 75 percent of the stomach is removed, leaving a narrow gastric tube or “sleeve.” No intestines are removed or bypassed during the procedure and it takes about one to two hours to complete. When compared to the gastric bypass, the LSG can offer a shorter operative time that can be an advantage for patients with severe heart or lung disease.
Weight-loss:
The LSG procedure greatly reduces the size of the stomach and limits the amount of food that can be eaten at one time. It does not cause decreased absorption of nutrients or bypass the intestines. After this surgery, patients feel full after eating very small amounts of food. LSG may also cause a decrease in appetite. On average, by year three, sleeve patients lost approximately 21 percent of their total body weight (weight at time of procedure). In a 350 pound person, this would mean a 74 pound weight-loss.
Gastric Bypass
Gastric bypass surgery, also called Roux-en-Y gastric bypass, has two parts. First, the surgeon staples your stomach, creating a small pouch in the upper section. The staples make your stomach much smaller, so you eat less and feel full sooner.
Next, the surgeon cuts your small intestine and attaches the lower part of it directly to the s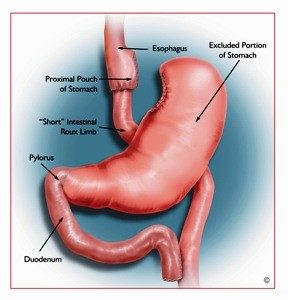 mall stomach pouch. Food then bypasses most of the stomach and the upper part of your small intestine so your body absorbs fewer calories. The surgeon connects the bypassed section farther down to the lower part of the small intestine. This bypassed section is still attached to the main part of your stomach, so digestive juices can move from your stomach and the first part of your small intestine into the lower part of your small intestine. The bypass also changes gut hormones, gut bacteria, and other factors that may affect appetite and metabolism. Gastric bypass is difficult to reverse, although a surgeon may do it if medically necessary.
mall stomach pouch. Food then bypasses most of the stomach and the upper part of your small intestine so your body absorbs fewer calories. The surgeon connects the bypassed section farther down to the lower part of the small intestine. This bypassed section is still attached to the main part of your stomach, so digestive juices can move from your stomach and the first part of your small intestine into the lower part of your small intestine. The bypass also changes gut hormones, gut bacteria, and other factors that may affect appetite and metabolism. Gastric bypass is difficult to reverse, although a surgeon may do it if medically necessary.
A gastric bypass can be done through a single long incision (open) or through a series of small incisions (laparoscopic). Regardless of how the operation is done, the “inside part” is the same.
The surgery involves three basic steps:
- Dividing the large stomach into two separate stomachs, thus creating a small pouch (proximal pouch of stomach) and a larger excluded lower pouch (remnant pouch of stomach)
- Bypassing part of the small intestine (creating the “Short” Intestinal Roux Limb)
- Attaching the bypassed intestine (Roux Limb) to the proximal pouch
The operation can usually be done in two hours or less, but this will depend on many factors. Most patients will need to stay in the hospital for two to three days after their operation and should be ready to return to full activity within two weeks.
Weight-loss:
On average, by year one, bypass patients lost approximately 34 percent of their total body weight (weight at time of procedure). In a 350 pound person, this would mean a 119 pound weight-loss. By year three, bypass patients lost approximately 31.5 percent of their total body weight (weight at time of procedure).
Duodenal Switch
This surgery, also called biliopancreatic diversion with duodenal switch, is more complex than the others. The duodenal switch involves two separate surgeries. The first is similar to gastric sleeve surgery. The second surgery redirects food to bypass most of your small intestine. The surgeon also reattaches the bypassed section to the last part of the small intestine, allowing digestive juices to mix with food.
This type of surgery allows you to lose more weight than the other three. However, this surgery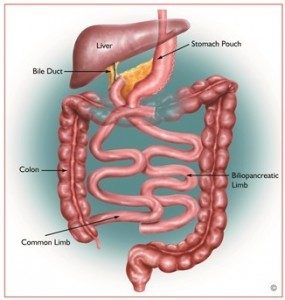 is also the most likely to cause surgery-related problems and a shortage of vitamins, minerals, and protein in your body. For these reasons, surgeons do not perform this surgery as often.
is also the most likely to cause surgery-related problems and a shortage of vitamins, minerals, and protein in your body. For these reasons, surgeons do not perform this surgery as often.
The outer margin of the stomach is removed (approximately two thirds—similar to a sleeve gastrectomy) and the intestines are then rearranged so that the area where the food mixes with the digestive juices is short.
A portion of the stomach is then left with the pylorus still attached and the duodenum beginning at its end. The duodenum is then divided, allowing for the pancreatic and bile drainage to be bypassed. It is a pyloric saving procedure, which eliminates the “dumping syndrome” that is inherent to gastric bypass.
Weight-loss:
This procedure results in decreased absorption of fat, calories and other nutrients which may result in increased weight-loss. Foods high in fat content are not easily absorbed and will be eliminated along with the usually high calories associated with the high-fat. On average, by year three, BPD/DS patients lost approximately 35 percent of their total body weight (weight at time of procedure). In a 350 pound person, this would mean a 123 pound weight-loss.
In all bariatric surgery procedures, carbohydrates and sugars are absorbed, so eating foods high in sugar (and calories) will still cause unwanted weight gain or difficulty to lose weight. Additionally, emphasis is placed on nutritionally beneficial and nutrient dense foods. The BPD/DS allows patients to increase portion size throughout, allowing for greater diversity in food consumption at each meal.
Before Surgery
- The doctor will ask about your medical history, do a thorough physical exam, and order blood tests. If you are a smoker, he or she will likely ask you to stop smokingat least 6 weeks before your surgery.
- The surgeon will tell you more about the surgery, including how to prepare for it and what type of follow-up you will need.
- The dietician will explain what and how much you will be able to eat and drink after surgery and help you to prepare for how your life will change after surgery.
- The psychiatrist or psychologist may do an assessment to see if bariatric surgery is an option for you.
After Surgery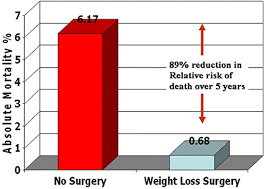
After surgery, you will need to rest and recover. Although the type of follow-up varies by type of surgery, you will need to take supplements that your doctor prescribes to make sure you are getting enough vitamins and minerals.
Walking and moving around the house may help you recover more quickly. Start slowly and follow your doctor’s advice about the type of physical activity you can do safely. As you feel more comfortable, add more physical activity.
How much weight can I expect to lose?
The amount of weight people lose after bariatric surgery depends on the individual and on the type of surgery he or she had. A study following people for 3 years after surgery found that those who had gastric band surgery lost an average of about 45 pounds. People who had gastric bypass lost an average of 90 pounds. Most people regained some weight over time, but weight regain was usually small compared to their initial weight loss.
Researchers know less about the long-term results of gastric sleeve surgery, but the amount of weight loss seems to be similar to or slightly less than gastric bypass.
Your weight loss could be different. Remember, reaching your goal depends not just on the surgery but also on sticking with healthy lifestyle habits throughout your life.
