Introduction(overview):
The mastoid, along with the tympanic, squamous, and petrous bones, forms the temporal bone. A number of critical structures are either located within or traverse through the temporal bone. The temporal bone is located between the occipital bone posteriorly, the parietal bone superiorly, the sphenoid bone anterior-medially, and the soft tissues of the neck inferiorly. The mastoid has a cortical osseous covering of varying thickness and is filled with very thin osseous septations, which form an air cell system similar in appearance to the ethmoid paranasal sinus.
Successful and safe mastoid surgery requires routine identification of key anatomic structures including but not limited to the tegmen (middle fossa floor), sigmoid sinus, external auditory canal, lateral semicircular canal, and facial nerve.
A high-speed electric or pneumatic drill with various tools and attachments are used in conjunction with copious suction irrigation when performing mastoid surgery. Adequate irrigation serves to wash away bone dust generated by the drill to improve visualization.
What is Mastoidectomy?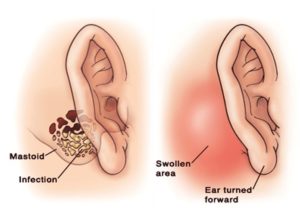
A mastoidectomy is a surgical procedure that removes diseased mastoid air cells. The mastoid is the part of your skull located behind your ear. It’s filled with air cells made of bone and looks like a honeycomb. The diseased cells are often the result of an ear infection that has spread into your skull. The procedure can also be used to remove an abnormal growth of the ear known as a cholesteatoma.
There are variations of mastoidectomy procedures, including:
- Simple mastoidectomy, in which your surgeon opens your mastoid bone, removes the infected air cells and drains your middle ear
- Radical mastoidectomy, in which your surgeon may remove your mastoid air cells, your eardrum, most of your middle ear structures, and your ear canal. This procedure is reserved for the complicated mastoid disease.
- Modified radical mastoidectomy, which is a less severe form of radical mastoidectomy that involves removing mastoid air cells along with some, but not all, middle ear structures
You can expect some hearing loss from a radical and modified radical mastoidectomy.
Why Mastoidectomy?
A mastoidectomy can treat complications of chronic otitis media (COM). COM is an ongoing ear infection in your middle ear. A cholesteatoma, which is a skin cyst, can be a complication from these ongoing infections. The cyst grows gradually over time and may lead to serious complications such as:
- abscess in the brain
- deafness
- dizziness or vertigo
- damage to your facial nerve that causes facial paralysis
- meningitis, or inflammation of the membranes of your brain
- labyrinthitis, or inflammation of your inner ear
- ongoing ear drainage
Your doctor may also perform a mastoidectomy to put in a cochlear implant. This small, complex electronic device can help provide you with a sense of sound if you’re profoundly deaf or severely hard of hearing.
This surgery can also remove abnormal growths at the base of your skull.
Chronic otitis media (COM)with or without cholesteatoma, is one of the more common indications for performing a mastoidectomy. Patients with chronic otitis media often present with otorrhea and progressive hearing loss. Mastoidectomy permits access to remove cholesteatoma matrix or diseased air cells. In addition, mastoidectomy often provides access to the temporal bone which is more challenging to visualize through the external auditory canal (ie, supernatural recess, epitympanum, facial recess, peri labyrinthine air cells, retro facial hair cells).
Mastoidectomy is one of the key steps in placing a cochlear implant to rehabilitate acquired or congenital sensorineural hearing loss. A mastoidectomy allows the surgeon access to the middle ear through the facial recess. The implant electrode array is placed through the facial recess into a cochleostomy, which is drilled inferior and slightly anterior to the round window.
A mastoidectomy is often an initial step in the removal of lateral skull base neoplasms, including vestibular schwannomas, meningiomas, temporal bone paragangliomas (glomus tumors), and epidermoids.
Complications of otitis media, including intertemporal or intracranial suppuration and lateral venous sinus thrombosis, often necessitate a mastoidectomy.
How is it performed?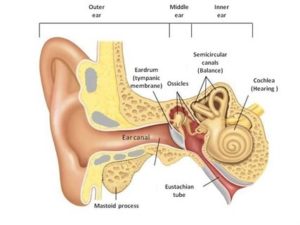
Your doctor usually performs a mastoidectomy using general anesthesia. This ensures that you’re asleep and unable to feel pain. For a simple mastoidectomy, your surgeon will usually:
- Access your mastoid bone through a cut made behind your ear.
- Use a microscope and a small drill to open your mastoid bone.
- Use suction irrigation to keep the surgical area free of bone dust.
- Drill out the infected air cells.
- Stitch up the operative site.
- Cover the site with gauze to keep the wound clean and dry.
- Your surgeon may also use a facial nerve monitor during surgery. This helps to limit injury to the facial nerve.
Procedure in detail:
- Anesthesia:
Mastoidectomy procedures are typically performed under general anesthesia.The use of long-acting paralytics is not recommended because this does not allow the surgeon to assess the function of the facial nerve, either through a hand-held stimulator or a nerve integrity monitor.
The planned postauricular incision area is typically infiltrated with lidocaine or Marcaine with diluted epinephrine from the region of the mastoid tip up to the linea temporalis. Infiltration of the ear canal is also necessary in most cases to decrease bleeding. Some surgeons use diluted epinephrine without anesthetic because this injected solution sometimes migrates into the middle ear in the vicinity of the facial nerve and may negate the benefits of facial nerve monitoring.
- Equipment:
An operating microscope with a 200-250 mm objective is used for either the entire procedure or once the superficial drilling has been completed. A number of microscopes are available, which are specifically designed for otologic surgery.
An otologic drill with various tools and attachments, including cutting and diamond burrs, is used for all mastoid surgery. Various manufacturers produce both pneumatic and electric otologic drills. The foot pedal may be controlled by the surgeon or the surgical technician, depending on surgeon preference. Initial bone removal is typically done with a large, round, fluted cutting burr. Burr size is progressively reduced as dissection proceeds medially into the temporal bone. A round diamond burr is typically used adjacent to critical structures to reduce the risk of injury.
Suction irrigators of various sizes allow the surgeon to rinse away bone dust to improve visualization and to reduce the risk of thermal injury from the drill.
Various microinstruments specifically designed for otologic surgery are used to dissect, elevate, remove, or transect structures in the temporal bone.
The facial nerve monitor does not eliminate the risk of a facial nerve injury during mastoid surgery. No substitute exists for thorough anatomic knowledge of the temporal bone in order to avoid complications, especially a facial nerve injury. Facial nerve monitoring can provide the surgeon with mechanical feedback during drilling and microdissection in the vicinity of the facial nerve. This feedback allows the surgeon to modify their technique intraoperatively, potentially avoiding an injury to the facial nerve. Paired electrodes are typically placed in the orbicular is and oculi and a ground electrode are placed on the forehead or upper chest. If the integrity of the facial nerve is a concern, a stimulating probe can be used to confirm the anatomic and physiologic integrity of the nerve. [4]
- Positioning:
The patient is almost always placed in the supine position with the head rotated approximately 30-45 º away from the surgeon, depending on the patient’s neck range of motion. Careful communication with the anesthesia provider is important because, after induction, the patient is typically rotated 180 º. Positioning the patient’s head as close to the edge of the bed adjacent to the surgeon provides an ideal working distance for the surgeon. The patient’s head is typically positioned at the foot of the bed so the surgeon can have their legs under the operating room table while sitting.
After the surgery?
You can expect to have bandages over your ear when you wake up. There will also be stitches close to your ear. You may have a headache, discomfort, and some numbness.
After surgery, your doctor may:
- prescribe pain medication
- give you antibiotics to treat any infection
- ask you to schedule a return for wound check and removal of any bandages and stitches
Follow your doctor’s specific instructions on caring for your wound, as well when you can swim or bathe. You should avoid all strenuous activity for at least two to four weeks afterward, depending on your surgery. Also, refrain from putting pressure on your ear.
Patients commonly are up and about on the evening of the day of surgery and usually are discharged from the hospital on the day following surgery. Following mastoidectomy, it may be necessary to perform a minor skin graft procedure called a Thiersch graft. A transparent layer of skin is removed from the inside part of the upper arm and is placed over the surgical area inside the ear. This aids in the healing process and protects the ear from infection. If this is necessary, it is usually done in 10 to 30 days following the mastoidectomy. Patients will need appointments for ear cleanings at least twice yearly for the rest of their lives after mastoidectomy, as their ear will no longer be able to clean itself as normal ears do.
