Glaucoma and its Introduction:-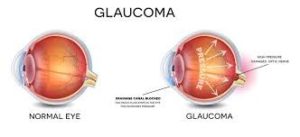
Glaucoma is a disease of the eye in which fluid pressure within the eye rises – if left untreated, the patient may lose vision and even become blind. The disease usually affects both eyes, although one may be more severely affected than the other.
There is a small space in the front of the eye called the anterior chamber. Clear liquid flows in and out of the anterior chamber; this fluid nourishes and bathes nearby tissues. If a patient has glaucoma, the fluid drains too slowly out of the eye. This leads to fluid build-up, and pressure inside the eye rises.
Unless this pressure is brought down and controlled, the optic nerve and other parts of the eye may become damaged, leading to loss of vision.
Glaucoma is one of the most common causes of legal blindness in the world. At first, people with glaucoma lose side (peripheral) vision. But if the disease isn’t treated, vision loss may get worse. This can lead to total blindness over time.
Types of glaucoma
There are two main types: open-angle and closed-angle glaucoma.
Closed-angle glaucoma (acute angle-closure glaucoma)
This can come on suddenly; the patient commonly experiences pain and rapid vision loss. Fortunately, the symptoms of pain and discomfort make the sufferer seek medical help, resulting in prompt treatment, which usually prevents any permanent damage from occurring.
Primary open-angle glaucoma (chronic glaucoma)
This type progresses very slowly. The patient may not feel any symptoms; even slight loss of vision may go unnoticed. In this type of glaucoma, many people do not get medical help until permanent damage has already occurred.
Low-tension glaucoma
This is a rare form of glaucoma that experts do not fully understand. Even though eye pressure is normal, optic nerve damage still occurs. It might be due to reduced blood supply to the optic nerve.
Pigmentary glaucoma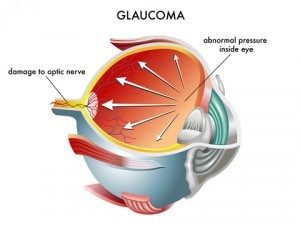
This is a type of open angle glaucoma and typically develops during early or middle adulthood. Pigment cells, which arise from the iris, are dispersed within the eye. If these cells build up in the channels that drain fluid from the eye, they can upset the normal flow of fluids in the eye, leading to a rise in eye pressure.
Causes of glaucoma
Experts are unsure of the precise causes of glaucoma, but cases are divided into two categories:
Primary glaucoma – this means that the cause is unknown.
Secondary glaucoma – the condition has a known cause, such as a tumour, diabetes, an advanced cataract, or inflammation.
There are several risk factors for glaucoma:
- Old age.
- Ethnic background – East Asians, African Americans, and those of Hispanic descent have a higher risk of developing glaucoma, compared with Caucasians.
Some illnesses and conditions – like diabetes or hypothyroidism.
- Eye injuries or conditions.
- Eye surgery.
- Myopia (nearsightedness).
Symptoms of Glaucoma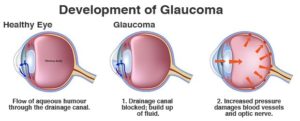
At first, there are no symptoms. Vision stays normal, and there is no pain.
However, as the disease progresses, a person with glaucoma may notice his or her side vision gradually failing. That is, objects in front may still be seen clearly, but objects to the side may be missed.
As glaucoma remains untreated, people may miss objects to the side and out of the corner of their eye. Without treatment, people with glaucoma will slowly lose their peripheral (side) vision. They seem to be looking through a tunnel. Over time, straight-ahead vision may decrease until no vision remains.
Glaucoma can develop in one or both eyes.
How is glaucoma detected?
Glaucoma is detected through a comprehensive eye exam that includes:
- Visual acuity test. This eye chart test measures how well you see at various distances. A tonometer measures pressure inside the eye to detect glaucoma.
- Visual field test. This test measures your side (peripheral) vision. It helps your eye care professional tell if you have lost side vision, a sign of glaucoma.
- Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Tonometry. An instrument (right) measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
- Pachymetry. A numbing drop is applied to your eye. Your eye care professional uses an ultrasonic wave instrument to measure the thickness of your cornea.
Risk Factors
Glaucoma is often called “the sneak thief of sight.” This is because, as already mentioned, in most cases, the intraocular pressure can build up and destroy sight without causing obvious symptoms. Thus, awareness and early detection of glaucoma are extremely important because this disease can usually be successfully treated when diagnosed early. While everyone is at risk for glaucoma, certain people are at a much higher risk and need to be checked more frequently by their eye doctor. The major risk factors for glaucoma include the following:
- Age over 45 years
- Family history of glaucoma
- Black racial ancestry
- Diabetes
- History of elevated intraocular pressure
- Decrease in corneal thickness and rigidity
- Nearsightedness (high degree of myopia), which is the inability to see distant objects clearly
- History of injury to the eye
- Use of cortisone (steroids), either in the eye or systemically (orally or injected)
- Farsightedness (hyperopic), which is seeing distant objects better than close ones (Farsighted people may have narrow drainage angles, which predispose them to acute [sudden] attacks of angle-closure glaucoma.)
Treatments for glaucoma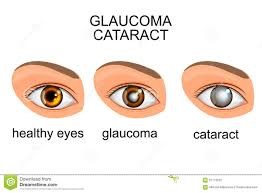
- Eye drops for glaucoma
- older man putting eye drops in his eye
- Eye drops are a common and effective treatment for
In the majority of cases, initial treatment for glaucoma includes eye drops.
Compliance is vital for best results and to prevent undesirable side affects – this means following the doctor’s instructions carefully.
Examples of eye drops include:
- prostaglandin analogues
- carbonic anhydrase inhibitors
- cholinergic agents
- beta blockers
Side effects of eye drops can include stinging, redness, eyelash growth, change in eye colour and occasionally retinal detachments and difficulty breathing. If eye drops are not effective enough, the doctor may prescribe an oral carbonic anhydrase inhibitor.
Side effects are less if they are taken during meals. Initial side effects can include tingling in the fingers and toes and frequent urination – however, after a few days, they usually resolve.
Much less commonly, there is a risk of rashes, kidney stones, stomach ache, weight loss, impotence, fatigue, and a strange taste when consuming fizzy drinks.
Surgery for glaucoma
If drugs don’t work, or if the patient cannot tolerate them, surgical intervention may be an option. The aim of surgery is usually to bring down the pressure inside the eye. Examples of surgery include:
- Trabeculoplasty – a laser beam is used to unblock clogged drainage canals, making it easier for the fluid inside the eye to drain out.
- Filtering surgery (viscocanalostomy) – this may be carried out if nothing else works, including laser surgery. Channels within the eye are opened up to improve fluid drainage.
- Drainage implant (aqueous shunt implant) – this option is sometimes used for children or those with secondary glaucoma. A small silicone tube is inserted into the eye to help it drain out fluids better.
Acute angle-closure glaucoma
Acute angle-closure glaucoma is treated as a medical emergency. Pressure-reducing medications are administered immediately. A laser procedure is usually carried out that creates a tiny hole in the iris, allowing fluids to pass into the trabecular meshwork (the drainage system of the eye) – this procedure is called an iridotomy.
Even if only one eye is affected, the doctor may decide to treat both, because this type of glaucoma often affects the other eye, too.
Deciding about surgery
Deciding whether to have surgery is difficult because:
- You may not be in pain or notice any vision loss.
- Your vision may get worse right after surgery and may be affected for weeks or months. Your eyesight may not be as good as it was before the surgery.
- Surgery isn’t a complete cure for glaucoma. But surgery can decrease the chance of losing even more eyesight later on. And for some people, it can reduce or get rid of the need for eye drops.
- Not everyone who has laser surgery will have lower IOP after the surgery. For most people, the lower pressure will last only a few years. Others may have an increase in their eye pressure. Certain types of open-angle glaucoma respond better to laser surgery than others.
- The effects of some laser treatments aren’t long-lasting. Repeat laser treatments, medicines, or other surgeries may be needed later on.
- As with any other surgery, you and your doctor should make the decision to operate based on the risks and benefits of having the surgery. One thing to consider is which eye should be operated on first. There may be other questions about glaucoma surgery that you should discuss with your doctor before making a decision.
- Cataracts may occur in people who also have glaucoma. This commonly occurs in older people. Surgery to remove the cataract may be done at the same time as surgery for glaucoma. If surgeries for glaucoma and a cataract are done at the same time, you may notice improved eyesight after surgery.
Prognosis for glaucoma
The prognosis for glaucoma depends on when the disease is detected. If the diagnosis is made before significant optic nerve damage occurs, the prognosis is generally good if the patient is compliant with the treatment suggested by the ophthalmologist. Since optic nerve damage is permanent and previously damaged optic nerves are more prone to additional damage, a delayed diagnosis (one made after significant optic nerve damage and field loss has already occurred) requires more aggressive therapy and carries a prognosis for future visual loss, which is guarded over the long term.
Prevention of Glaucoma
Most of the risk factors (such as age, race, and family history) for glaucoma are beyond your control. Whether or not you are at increased risk for glaucoma, it’s best to get routine eye exams and tests as your eye doctor suggests. Finding and treating glaucoma early is important to help prevent blindness.
If you have high pressure in your eyes but you don’t have glaucoma, your eye doctor may suggest treatment that helps lower your eye pressure. This may help delay or prevent the onset of glaucoma.
Future of Glaucoma
New eye drops will continue to become available for the treatment of glaucoma. Some drops will be new classes of agents. Other drops will combine some already existing agents into one bottle to achieve an additive effect and to make it easier and more economical for patients to take their medication.
